By: Dr. Shawn Meirovici N.D.
Intro
As a cannabis educator and naturopathic doctor I naturally get asked several questions about cannabis. Specifically cannabidiol (CBD) and epilepsy. I believe CBD enriched cannabis oil can be an effective and safe first or second line therapy for various forms of epilepsy and this is why.
Back Story on CBD and Epilepsy
Allow me to first tell you a bit about the story behind CBD and epilepsy. The potential of CBD as a therapeutic option in treating epilepsy came to the forefront back in 2013. Renowned CNN medical journalist Dr. Sanjay Gupta did a special report series on cannabis called “Weed”. One of these episodes highlighted a 5 year old girl named Charlotte Figi.
Charlotte, who had been diagnosed with a severe form of epilepsy called Dravet Syndrome, was being treated with a concentrated CBD oil. Dravet syndrome is characterized by prolonged and frequent seizures that typically begin in the first year of life. Without successful treatment, Dravet can lead to severe health concerns including developmental disabilities. After several anti-epileptic drugs failed to control her seizures, Charlottes family had began to research alternative options to help their daughter.
A little known fact is that CBD was actually discovered and researched before the most famous of the cannabinoids, delta-9 tetrahydrocannabinol (THC). Not too long after the discovery of CBD, research into the calming effects of CBD on the neurological system and its potential as an anti-epileptic came to surface.
One such study came from the Journal of Clinical Pharmacology. Published in 1981, the study found that cannabidiol was effective in almost all epileptic patients (secondary generalized epilepsy) at a dose of 200-300mg daily for 4.5 months. There were no psychological or physical symptoms suggestive of psychotropic or toxic effects. (1)
The Figi’s soon came across some of this research and began searching for high CBD strains of cannabis (not easily attainable at the time). They came across the Stanley Brothers in Colorado who had bred a high CBD low THC strain of marijuana known as “Hippie’s Disappointment”. The name suggesting its low THC content and little to no psychotropic effects.
Charlottes parents and physician said that she experienced a reduction of her epileptic seizures after her first dose of CBD oil! The strain was then renamed “Charlotte’s Web” and thus began a flurry of interest into cannibidiol and changing of marijuana laws across America.
More recently there have been several high quality clinical trials, including three phase 3 clinical trials in 2017. These trials demonstrated the efficacy of cannabidiol in reducing convulsive seizure activity; specifically in children with treatment-resistant Dravet syndrome and Lennox-Gastaut syndrome. (2)

Dr. Sanjay Gupta M.D. CNN Special Report “Weed”
How CBD works
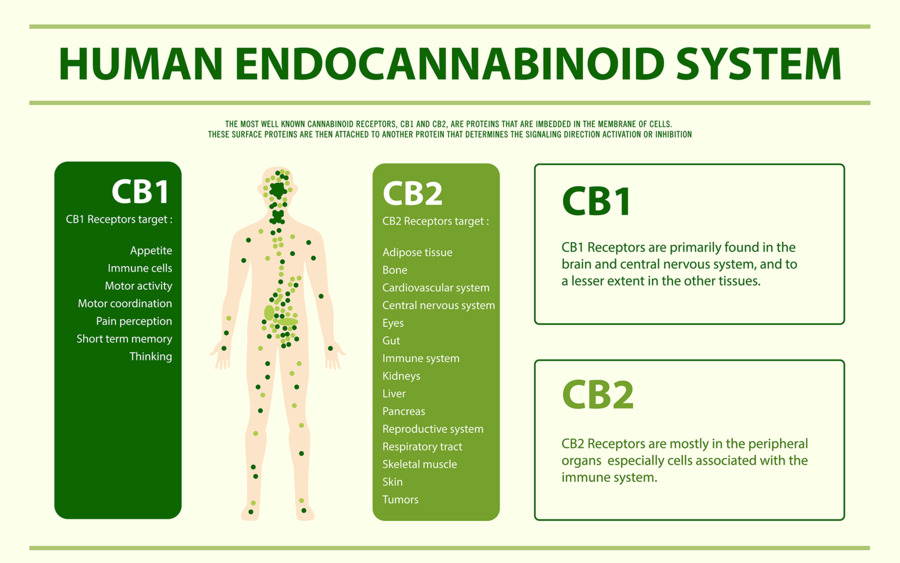
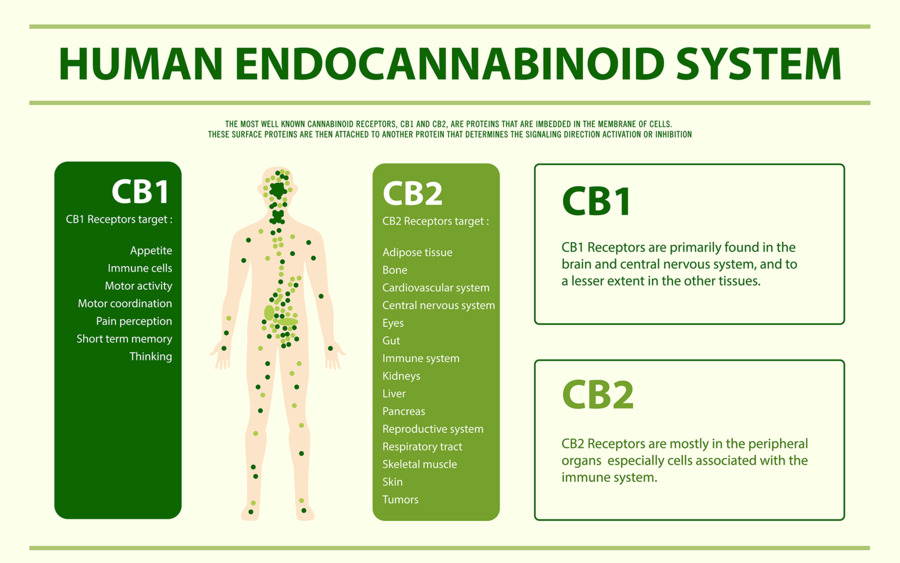
I will now explain how we think CBD works in convulsive syndromes. In order to do so I must first briefly explain an important biological system that all humans, in fact all creatures with the exception of insects, possess called the Endocannabinoid System (ECS). The ECS regulates many bodily systems to maintain balance. One such job of the ECS is to function as a self-regulating harm reduction system; essentially acting as a breaker system shutting down power when circuits get overloaded.
The ECS is able to do this via chemical messengers in our body called endocannabinoids (Cannabinoids found within our body). The two main endocannabinoids are Anandamide (AEA) and 2-Arachidonoylglycerol (2-AG). Endocannabinoids are released at the postsynaptic neuron (the receiving end of a chemical signal). Through retrograde inhibition (a feedback loop) can turn off or quiet a signal. As you can imagine, if there was no off switch things would go haywire very quickly.
Circling back to epilepsy, one of the ways the ECS functions is by maintaining homeostasis in the nervous system. The ECS is involved in the prevention of excess neuronal activity as is the case with a convulsive seizure. So you may now be wondering how CBD fits into this picture.
Our ECS is activated via receptors called cannabinoid receptors. We have many types of these receptors throughout our body. Our endocannabinoids (AEA and 2-AG) as well as phytocannabinoids (cannabinoids from plants such as THC) activate these receptors. Unlike THC, however, CBD does not fit well into our cannabinoid receptors. CBD instead boosts the activity of our endocannabinoids (AEA and 2-AG) by slowing their enzymatic breakdown.
In short, CBD can increase our endocannabinoid tone by inhibiting re-uptake. Much like how an antidepressant boosts serotonin activity by inhibiting re-uptake of serotonin.
There are many other physiological actions of CBD, such as being a potent anti inflammatory and having antidepressant effect. However, for the purposes of understanding how it can work in epilepsy, CBD is thought to act by increasing endocannabinoid tone in the nervous system.
CBD is regarded as a very safe medicinal substance as it doesn’t directly stimulate our receptors, as do many other drugs. Rather, it boosts our own innate endocannabinoid activity.
CBD Safety In Epilepsy
CBD is a generally well tolerated medication, and has no known toxicity (we’re not sure if its even possible to overdose from it). There are however some things that are important to point out to patients considering using CBD, especially when it comes to epileptic patients already taking other anti epileptic drugs (AED).
A randomized control trial (RCT) from 2018 in the journal of Neurology aimed to evaluate the safety of CBD in children with Dravet syndrome. The patients were aged 4-10 years and they received a CBD oil at relatively high doses (5, 10 or 20mg/kg/day). That equates to 65mg per day on the lower end and 260mg per day on the higher end for a 30lb child.
Considering the average adult using CBD consumes somewhere between 20-60mg per day, that’s a pretty hefty dose for a child. The results of the study indicated that for the most part CBD had no effect on other AEDs’ (Clobazam, Valproate, Levetiracetam, Topiramate and Stripentol). There was one exception with N-desmethylclobazam in which it increased levels of this drug. This effect is likely due to how CBD can slow down liver metabolism via a specific enzyme called CYP450. (3)
There was also an increase in liver enzymes in 6 patients taking both valproate and CBD. Something that may not be of much clinical significance but should be monitored. Most of my medicated patients with epilepsy are prescribed Keppra (Levetiracetam) as a first line therapy. It’s good to know that even at high doses (260mg/day) CBD is not likely to interact with this medication. Valproate is the second most common AED that I see clinically. In these patients it is recommended to test the liver enzymes every so often.
There were more adverse effects (AE) in those patients taking CBD as compared to placebo. The most common AEs’ being pyrexia, somnolence, decreased appetite, sedation, vomiting, ataxia and abnormal behaviour. In general CBD was well-tolerated. To compare, the most common AEs’ in patients taking Keppra (Levetiracetam) are: headache, increased blood pressure, somnolence, drowsiness, fatigue, anorexia, weakness, nasopharyngitis and cough. Keppra is also one of the more well tolerated AEDs’. In my opinion CBD, at the very least, is very similar to Keppra in safety profile and efficacy and should therefore be considered as a first or second line therapy.


CBD Efficacy in Epilepsy
One of the more recent studies looking into CBD and epilepsy was conducted just down the street from me at the Hospital for Sick Kids (a world renowned children’s hospital in Toronto Canada).
The study was published in the Annals of Clinical Translational Neurology in August of 2018. What was even more exciting is that the study used a CBD enriched cannabis oil from a licensed producer (Tilray) that many of my patients have access to. The CBD oil contained 100mg/ml CBD and 2mg/ml THC. Nineteen children with Dravet syndrome received the CBD oil for the complete 20-week intervention. The average dose was 13.3mg/kg/day (right in line with the dose of previously discussed safety study). The most common AEs’ were: somnolence, anorexia and diarrhea. Liver enzymes increased in patients also taking Valproate (so it looks like the interactions and adverse effects are pretty consistent).
There was a statistically significant improvement in quality of life, reduction in EEG spike activity (correlated with seizure activity), an average motor seizure reduction of 70.6% (motor seizure reduction rate in Keppra is around 37%) with a 50% responder rate of 63% (comparable to Keppra). (4)(5) Click Here for Sick Kids Study

CBD as first line therapy in Epilepsy
At this point you may be wondering why CBD is not generally considered as a first line therapy option for convulsive seizure disorders?
The reality is that the medical system in North America is generally very conservative in accepting new treatments. This is often a good thing (protecting the public from potentially dangerous or useless medications). However, on the flip side it can be a obstacle for getting naturally derived medicines, that we know to be safe and likely effective, to the patients that would benefit from them.
Currently we only have studies using CBD oil or CBD enriched cannabis oil (Containing other cannabinoids like THC) in patients with severe forms of epilepsy, or who have failed to see benefit with several other AEDs’. However, if we take into account all the information we do have on CBD, we can draw some pretty solid conclusions about its safety profile, the potential adverse effects, interactions with other drugs and its efficacy.
Until we see a robust amount of research using CBD as a first line therapy in a wider array of seizure disorders it is not likely to be accepted as a first or second or third choice by many neurologists. As a Naturopathic Doctor and cannabis educator I do see the potential of CBD for epilepsy. I will therefore continue to advocate for CBDs’ consideration as a first or second line therapeutic agent in many of my patients with epilepsy.
Check out my other articles on CBD and medical marijuana
Epilepsy Foundation stance on medical marijuana

References
- Carlini EA, Cunha JM. Hypnotic and antiepileptic effects of cannabidiol. J Clin Pharmacol. 1981;21(S1):417S-427S. doi:10.1002/j.1552-4604.1981.tb02622.x
- O’Connell, Brooke (May 1, 2017), “Cannabinoids in treatment-resistant epilepsy: A review.”, Epilepsy Behav, Epilepsy & Behavior, 70, 6, 341-348, 70: 341–348, doi:10.1016/j.yebeh.2016.11.012, PMID 28188044
- Devinsky O, Patel AD, Thiele EA, et al. Randomized, dose-ranging safety trial of cannabidiol in Dravet syndrome. Neurology. 2018;90(14):e1204-e1211. doi:10.1212/WNL.0000000000005254
- McCoy B, Wang L, Zak M, et al. A prospective open-label trial of a CBD/THC cannabis oil in dravet syndrome. Ann Clin Transl Neurol. 2018;5(9):1077-1088. Published 2018 Aug 1. doi:10.1002/acn3.621
- Abou-Khalil B. Levetiracetam in the treatment of epilepsy. Neuropsychiatr Dis Treat. 2008;4(3):507-523. doi:10.2147/ndt.s2937
My review of Aurora Cannabis MK ULTRA 4.5 stars out of 5!
Why get a license?
I want to tell you how to obtain a license for Medical Marijuana. Every month I see a handful of patients who are trying to medicate with unregulated cannabis obtained either through “a guy” or a local illegal dispensary. The problem with this approach is that you are buying an unregulated product, meaning you cannot guarantee its purity, quality, potency, and cannabinoid profile.
There are some decent products out there but largely its hit and miss and perhaps the most frequent complaint is a lack of consistency from batch to batch. Its funny how patients will be shy about discussing use of medical marijuana with me and yet will go to a complete stranger for their medication. A growing part of my practice is convincing patients to transition from their “street weed” to a proper regulated medical marijuana product.
Although, as a Naturopathic Doctor, I am not able to directly prescribe medical marijuana in Ontario, I am fortunate to have a good professional relationship with a licensing clinic and am writing an average of 3-5 patient referrals per week. Most licensing clinics will require a referral from a healthcare professional.
How to get a license
The process is quite simple: a patient will come in either having experience with cannabis or will be curious as to whether cannabis can help them. I will then preform an assessment, including a health history and short physical exam, in order to determine if they would benefit from cannabis. A referral is then made to the licensing clinic. The licensing clinic then calls the patient to setup an appointment to get a license for access to medical marijuana. Once setup with an account the patient then does all their ordering online through a regulated distributor such as Tweed, Aphria, Tilray or MedRelief.
These regulated grower/distributors have an excellent selection of strains and oils with varying cannabinoid concentrations and terpene profiles. Most importantly, the purity and potency are guaranteed and there is very high consistency from batch to batch. Therefore, if you find a strain or oil that works for you, you can pretty much guarantee it will work the same way every time you order it.
Common conditions for referral
The most common conditions I write referrals for are: Insomnia, Multiple Sclerosis, Chronic Pain, Migraine, Irritable Bowel Syndrome, PTSD, Inflammatory Bowel Disease, Cancer, Fibromyalgia and Neurological Conditions with painful spasms.
The environment in Canada with regard to cannabis is going to change as we approach legalization, but until that happens I would advise you that it is usually better to consume regulated medicines, this medication just happens to be marijuana.
For more great articles and information on cannabis and CBD check out the link below:
How to Cook With Cannabis
Dr. Shawn demonstrates how to make edibles with medical marijuana. He’s talking CBD, THC, Terpenes, Cannabutter, Brownies and Pancakes.
Check out this “highly” informative instructional video.
Clinical Endocannabinoid Deficiency
Clinical endocannabinoid deficiency, (CED), was first introduced by Dr. Ethan Russo M.D. a neurologist, psychopharmacology researcher and former advisor to GW pharmaceuticals. The theory of CED is based on the concept that many neurological conditions are associated with neurotransmitter deficiencies, for example, a deficiency in dopamine with Parkinson’s disease. Subsequently, an endocannabinoid deficiency might be present in some disorders sharing predictable clinical features.
All humans possess an underlining endocannabinoid system governed by two primary compounds; Anandamide (AEA) and 2-Arachidonoylglycerol (2-AG). These are compounds naturally made in our body that interact with the same receptors marijuana and associated cannabinoids act upon. It is known through various studies that when endocannabinoid tone is decrease there is a lower pain threshold, disrupted digestion, mood and sleep disturbances. A deficiency of endocannabinoids can be caused by genetics, injury or disease.
Migraine
There is evidence for CED in several treatment resistant syndromes, most notably in Migraine, Fibromyalgia and Irritable Bowel Syndrome. All three present with: heightened pain sensitivity, mood disruption, and comorbidities. One study in chronic migraine sufferers discovered a statistically significant difference in endocannabinoid concentration within the cerebral spinal fluid of chronic migraine sufferers vs. non-migraine sufferers. With migraine there is a strong association between endocannabinoids and blood vessel dilation, a key component of the propagation of migraine. Furthermore activation of the CB1 cannabinoid receptor decreases pain fiber activity in the sensory nerves of the face and head.
It is worth noting that Cannabis was a mainstay treatment of migraine for a century between 1843 and 1943. A study from 2016 looked at the effects of medical marijuana on migraine headache frequency in adults. Headaches diminished from 10.4 to 4.6 attacks per month and overall 85.1% had decreased migraine frequency.
Fibromyalgia
Much like Migraine, Fibromyalgia is associated with hyperalgesia. In an uncontrolled trial of nine patients Tetrahydrocannabinol (THC) was administered in doses of 2.5-15mg a day for 3 months. Unfortunately 5 patients left the study early due to secondary THC side effects but those completing had marked reductions in subjective pain visual analog scales (VAS) 8.1 at start to 2.8 after 3 months. A survey of 1300 respondents called the National Pain Report from 2014 demonstrated that marijuana was the most effective treatment for Fibromyalgia compared to Duloxetine, Pregabalin and Milnacipran.
Irritable Bowel Syndrome
Another syndrome suspected of CED is Irritable Bowel Syndrome (IBS). The role of the endocannabinoid system in the gut is to regulate propulsion, secretion and inflammation. Cannabis was one of the first medications used for secretory diarrhea associated with cholera. A study done in 2007 demonstrated that endocannabinoids AEA and 2-AG influences the contractile force in the muscle fibers of the gastrointestinal tract. Studies also have demonstrated that there are increased levels of immunoreactive nerve fibers (TRPV1) causing pain and hypersensitivity in IBS. Cannabidiol (CBD) seems to increase AEA, which in turn reduces the activity of TRPV1. In 2007 a randomized control trial of 52 normal patients were given a single dose of 7.5mg THC. The outcome on the gastrointestinal tract was increased colonic compliance, inhibited postprandial tone, and a trend toward relaxation of fasting colonic tone.
There are a number of other conditions demonstrating evidence for CED, including motion sickness, Multiple Sclerosis, Huntington’s disease, Parkinson’s disease and Post Traumatic Stress Disorder (PTSD).
Conclusion
There is good evidence for disruption of the endocannabinoid system in Migraine, Fibromyalgia, IBS and many other neurological and psychiatric syndromes. Besides a wealth of anecdotal benefit, there exists some clinical evidence to support cannabinoids as a safe and effective treatment in these conditions. We also need to come to terms with the fact that effective medications are lacking in these conditions. An obvious shortcoming of past studies is the use of single cannabinoids for treatment such as THC. I am certain that future studies incorporating a more complete cannabinoid profile, including CBD, as a treatment approach will have far better outcomes and far fewer side effects. Lifestyle choices also play an important role in endocannabinoid function, specifically low-impact aerobic exercise. Multimodal approaches including diet, lifestyle and cannabinoid therapy will ultimately be the best approach in CED syndromes.
At my clinic I have repeatedly seen the benefits of cannabinoid therapy in these syndromes. After an initial assessment, if indicated, patients are referred to a medical cannabis clinic for registration under a licensed producer under the Access to Cannabis for Medical Purposes Regulations (ACMPR).
THC and CBD the ABC’s of Medical Marijuana
The perspective of a Naturopathic Doctor
As a practicing Naturopathic Doctor, I have understandably been occupying a front row seat in what has become one of today’s hot topic health issues; the use of medical marijuana. I have seen a trend recently in my patients; they’re dropping the conventional pain medications and experimenting with the unquestionably still taboo, cannabis. Two things seem to be driving this phenomenon: traditional pain medications aren’t doing the trick anymore and there is a curiosity about this promising although misunderstood plant.
Professionally, I too have been very curious about the medical applications of marijuana. For years patients would confide in me and share their experiences with using different preparations of cannabis. One of the usual preparations is “hemp oil”, which can contain a significant amount of a cannabinoid called CBD. Hemp oil may have been dismissed as folk remedy; however, with the recent surge in medical marijuana use prompting an educated examination of a potential effective therapy. I can now appreciate that hemp oil is a way to reap the benefits of cannabis without getting intoxicated.
There are thousands of articles on the web that explain in depth what the different components of marijuana are and how they differ in pharmacology and therapeutic applications. The point of this article is not to give a thesis but rather present a concise easy to grasp understanding of what those components do in the body and why cannabis in one form or another should be considered as a first choice medicine.
Before presenting the different types and components of marijuana, I would like to give this article some context and legitimacy by introducing myself, and my medical background. I am a Naturopathic Doctor and have been in private practice for just over 7 years in Toronto Canada. Over the past 4 years my practice has focused on the treatment of pain, debilitating neurological conditions and cancer. This really sets the stage as the first few regulated cannabis medications in Canada, namely Nabilone and Sativex, were approved for neuropathic pain, spasticity and nausea associated with cancer treatment and multiple sclerosis; both of which I see more consistently than the average naturopathic doctor. Naturally I started having patients that had experience with these medications or who were experimenting with unregulated forms of cannabis.
A watershed moment in my practice occurred when I began treating a 10-year-old girl that had suffered a stroke. I thought she would benefit from cannabis but at the same time was hesitant about subjecting her to the hallucinogenic properties of THC. Fortuitously around that very same time I viewed a CNN Sanjay Gupta report about a low THC / high CBD strain of marijuana called “charlottes web”. Treatment with this strain had been helping a young girl with a rare debilitating condition associated with frequent seizures. My young patient didn’t have seizures but had chronic high muscle tone as is also seen during seizures. The report also mentioned how CBD is not hallucinogenic. I was certainly intrigued as to the potential efficacy of this treatment and devoted both time and resources in understanding medical cannabis and CBD. As a result of this study and promising results, I now recommend CBD regularly in my practice. Now let’s take a step back and understand what CBD is and what does it do.
Although there are thousands of potentially therapeutic compounds in cannabis, research has really focused on two: THC and CBD. Depending on the sex and strain of the cannabis some will be higher or lower in one compound than the other.
THC is what gets you high. It acts on cannabinoid receptors in the body and brain with the result of inducing the perception altering experience that marijuana is known for. Along with the “high”, research has pointed out that there are definite pain lowering and mood enhancing properties of THC. However; there are some concerns with THC as it may impact learning in the developing brain, may trigger a psychotic episode in individuals predisposed to schizophrenia and impacts the users ability to carry out daily living tasks such as operating machinery and driving.
CBD, on the other hand, is a non-psychoactive component of cannabis that can comprise up to 40% of the active cannabinoids in marijuana. Although large doses of CBD in my experience can induce an intense feeling of relaxation there are no perception altering effects from even the highest doses of CBD. Research into this curious compound has pointed out that rather than binding to cannabinoid receptors in the body, as does THC, CBD for the most part blocks activity at these receptors and exerts most of its effect at a receptor called 5-HT1a. The 5-HT1a-receptor is linked to serotonin activity.
The overall effect of CBD in the complicated milieu of the human body is that it is anti-inflammatory, mood enhancing, offers protection for the nervous system, promotes relaxation, anti-spasmodic and negates some of the unwanted side-effects of THC consumption. CBD has even been shown to prolong the beneficial effects of THC by increasing the body’s amount of cannabinoid receptors. Furthermore, there has yet to be any evidence for negative side effects or toxicity even at very high doses of CBD per day. CBD research is currently exploring promising therapeutic effect in epilepsy, dementia, migraine and cancer. So all in all it’s a pretty impressive compound.
Now you may be wondering; “how do I get CBD?” – do I need a prescription and is it legal? Technically in Canada any derivative of Marijuana including THC and CBD is classified as a schedule 2-drug and can only be legally obtained with a prescription from a medical doctor. Personally I find it frustrating that Naturopathic Doctors, who receive 4 years of training in botanical medicine, are restricted from prescribing marijuana (a botanical last time I checked) whereas the responsibility falls on medical doctors who typically have no training in prescribing botanical preparations. Fortunately hemp, which is part of the cannabis family, is high in CBD, low in THC and in some cases legal (The legality of the extraction depends on factors such as THC levels and what part of the plant is used).
There are now many companies which specialize in CBD preparations derived from hemp and do not require a prescription from a medical doctor. Unfortunately the CBD on the market continues to be a bit pricey per milligram ($1/10mg) since a therapeutic dose often starts at around 40mg all the way up to 200mg per day. Hopefully in the future we will start to see some higher potency, cheaper preparations of CBD.
As a Naturopathic Doctor, I offer the following personal and professional perspective to both botanical medicines as a whole and specifically CBD. Medicines derived from whole botanicals are a complex collection of thousands of compounds. Often we really only have an understanding of a few of those compounds and that is what disorients many practitioners, especially medical doctors. However, I believe we should appreciate the complexity of botanical medicines precisely because our own physiology is just as complex. Pharmaceutical preparations are very specific in their composition and action in the body. Our bodies are not built that way and that is why we often see side effects with pharmaceutical preparations.
Certainly I do not claim that there are no side effects with botanical medicines, but it is a fact that there are far fewer. Pharmaceutical medicines have a definite time and place in specific treatment but we should not be frightened to use botanical medicines because it is their complexity that often make them safer for prolonged use proving for a more balanced therapeutic effect.
During my relatively short period of recommending CBD, I have seen the benefits in: Pain, Sleep, Focus and Rigidity. I work with a great deal of patients who have suffered from neurological injuries (Spinal cord injury, brain injury, stroke) and neurological disease (Multiple Sclerosis, Transverse Myelitis, Chronic Regional Pain Syndrome, Migraine, Fibromyalgia). I have witnessed more than half of these clients taper down or completely come off of several pain medications including addictive opioid medications and manage their symptoms more effectively with a combination of THC and CBD.
I have a number of patients who after several years of insomnia return to a normal sleep pattern with a therapeutic program that includes CBD. Many of my clients with high tone and muscle rigidity experience a relaxation response within minutes of taking CBD. In fact patients will often take a dose of CBD during a treatment session and will see the effects immediately. I have several patients tell me that since starting CBD their thinking has been clearer. I even have one patient who has told me that her vision is clearer, which makes sense in the context of inflammation of the optic nerve often experienced in multiple sclerosis.
As a Naturopathic Doctor it is my job to be on top of the latest research and treatment-options within the realm of nutraceuticals, complimentary therapies and herbal medicines. CBD is an exciting new treatment option with an excellent safety profile, promising results and that fits in well with my patient population. I am proud to an advocate for medical marijuana and have made a commitment to continue to update my patients and peers as to my clinical experience with CBD.