Amid the buzz about health measurements, there’s one that’s quietly gaining recognition: the phase angle. It’s like a secret code that reveals the health and resilience of your cells, offering a fresh perspective on your body composition and overall wellness. Whether you’re battling a chronic condition or simply striving for your best health, understanding your phase angle could be a game-changer. It’s a bit like having a personal health detective, tracking changes in your cells and guiding you towards smarter choices for your treatment and lifestyle. Curious to learn more? Why not schedule a body composition scan and unlock the mystery of your phase angle?
Understanding phase angle: The basics
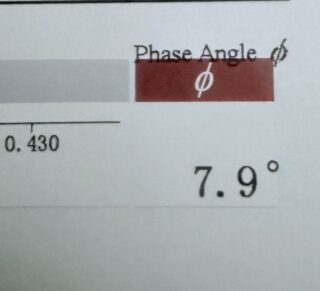
To get started, let’s talk about phase angle. It’s a measurement that captures the body’s electrical properties and provides a window into our cellular health. Phase angle is calculated through a method called bioelectrical impedance analysis (BIA). This non-invasive technique measures how our body tissues respond to a small electrical current, by looking at both resistance and reactance. Resistance is how much the body resists the current, and reactance is how much the body’s cell membranes resist the change in the current.
A higher phase angle is a good thing. It means that your cells are healthier and more resilient. In practical terms, a higher phase angle means you’re in better health. It can be a useful marker for a variety of health assessments. For example, it can help you see if your food and exercise programs are working by showing you how your cells are doing over time.
Phase angle changes can also tip us off to variations in body composition and fluid distribution. When our body’s water or the way fluids are spread between our cells and the rest of our body shifts, the phase angle will reflect that. This is why it’s a great tool for watching our water intake and catching any problems that could affect our overall health. And for healthcare pros and researchers, understanding these phase angle variations is key to getting a clearer picture of our physiological state.
But there’s more. Phase angle isn’t just about the basics. It’s proving to be a game-changer in how we manage chronic diseases and even approach cancer research. By giving us a number to track cellular health, it’s becoming a vital sign in treatment and nutritional monitoring. I’ll delve into these areas a bit later, but it’s worth noting now just how far-reaching the implications of phase angle are across the health spectrum.

How phase angle relates to body composition
Now that we know the basics, let’s talk about how phase angle can be a great way to see our body’s inner workings. It can show us how fat, muscle, and the overall health of our cells interact. Phase angle isn’t just a number; it’s a reflection of how robust and vibrant our cells are. It’s a measure we can thank bioelectrical impedance analysis (BIA) for, a non-invasive method that zaps a tiny electrical current through us to measure resistance and reactance. The phase angle, then, is the angle between these two measures, and it’s a goldmine of information about our cellular well-being.
Here’s the lowdown: a higher phase angle is like a high-five for your cellular well-being. It points to sturdy cell membranes and a well-hydrated cellular environment. And guess what? Your muscle mass is a big player in this game. Muscles, being the water and electrolyte havens they are, conduct electricity like champs. So, the more muscle you’ve got, the higher your phase angle is likely to be, reflecting a cellular landscape of robust health. On the flip side, lower phase angles might wave a red flag, hinting at cellular damage, inflammation, or dehydration—all the things we’d rather not have our cells dealing with.
I think this phase angle business is like a secret code our bodies are always sending. With the right tools, we can understand it to find a lot of information about our health. It’s like having a conversation with our cells, learning what they need to thrive. And let me tell you, the story they tell are pretty powerful. Over time, I’ve come to understand that a rising phase angle often means our cells are cheering, celebrating an upsurge in muscle mass or better hydration. But a dip in this angle? It’s a red flag, a signal that our cells might be struggling.
Keeping tabs on your phase angle is like having a secret window into your body’s inner workings. It’s a powerful tool for anyone looking to manage their health more effectively. Whether you’re working on your fitness, managing a chronic condition, or simply want to stay ahead of the game, phase angle can be your guide. It’s like having a trusted friend who knows you inside out, nudging you in the right direction to make the best choices for your health.

Phase angle in chronic disease management
It’s not just about the numbers on the scale or the percentages we see. The phase angle is a powerful tool in the fight against chronic disease, giving us a microscopic view of our cellular health and function. It’s based on bioelectrical impedance analysis (BIA) and tells us how well our body conducts electrical current. This is a direct reflection of our cell membranes’ integrity and function. In the fight against long-term disease, a higher phase angle is like a secret weapon. It shows better cell health and function, which can help us get better and recover.
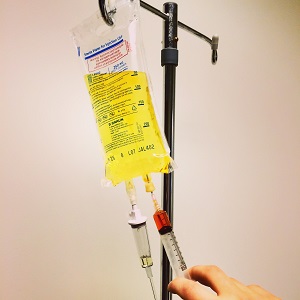
Let’s talk about diabetes. This is where phase angle steps up as a trusty sidekick, a biomarker that’s a game-changer for keeping tabs on your nutritional status and the health of your cells. Managing diabetes is a team effort, involving your diet, exercise, and any prescribed medications. But here’s the thing: by checking your phase angle often, your healthcare providers can see how healthy your cells are. This helps them make your treatment and diet plans better. A lower phase angle might tip them off that your cells need a little extra love, prompting them to adjust your care to keep you in the best shape possible.
And for those battling chronic heart failure, the phase angle is a beacon, predicting how the body might respond to treatments and even hinting at survival rates. With this condition, it’s not just the heart that’s at stake, but a whole symphony of organs and cells. A higher phase angle often whispers of a better response to therapies and a brighter chance at survival. For healthcare providers, it’s a compass, guiding them to adjust treatments and keep a vigilant eye on the disease’s dance.
Now, let’s talk about chronic kidney disease. It’s a tough one, and the phase angle is a big deal here, too. With chronic kidney disease, your cells can take a hit, and their function might not be as sharp as it once was. This can show up as lower phase angle values. But here’s the thing: studies have shown that higher phase angle values in these patients can mean better odds of making it through. So, by keeping an eye on phase angles, healthcare providers can get a clearer picture of what’s going on with their patients and make more informed decisions about their care.

The role of phase angle in cancer research
In cancer research, phase angle has become a bright spot. It gives us important clues that can help us diagnose, predict, and track treatments. One of the most significant findings is its link to cell membrane integrity. In the realm of cancer, this is no small matter, as the health of these membranes can greatly impact how cancer cells behave and respond to treatments. By peering into phase angle, we’re given a window into the cellular health of patients, a vital piece of the puzzle in crafting treatment plans that truly make a difference.
Research consistently tells us that lower phase angles are linked to less favorable outcomes for those battling cancer. It’s like a window into the health of our cells, and if that window is foggy, it can spell trouble. But here’s the thing—by keeping an eye on phase angle over time, we can get a clearer picture of how the disease is progressing and how our treatments are working. If we see that phase angle on the upswing, it’s a glimmer of hope, a sign that maybe, just maybe, our cells are rallying and we’re on the path to better days.
Moreover, studies have hinted that phase angle could be the crystal ball for how one might respond to chemotherapy. Imagine how powerful that would be. A healthcare provider with this knowledge could create a treatment plan that’s just right for you, which could make it more likely that you’ll get better. It’s about minimizing the guesswork and maximizing the benefits, all by understanding what’s happening at the cellular level.
And here’s something that’s really piqued my interest: the potential to boost phase angle through smart nutrition and targeted therapies. By shoring up the integrity of our cell membranes, we might just be able to bolster the health of those fighting cancer. This approach is all-encompassing. It not only treats the disease itself, but it also helps our body’s natural defenses, which may lead to better long-term results.
Improving health through phase angle analysis
With a deeper understanding of how phase angle is a health barometer, let’s explore how we can put this knowledge to work. One of the most remarkable things about this technology is its potential to catch chronic diseases in their earliest stages. Armed with this information, healthcare providers can act swiftly, halting the advance of the illness and improving patient well-being. Early detection is key, as it opens the door to personalized interventions that can make a world of difference in quality of life.
I’ve learned that higher phase angles often signal better cellular health, a key player in our overall well-being. When our cells are in top form, our bodies are better at fending off infections, bouncing back from illnesses, and maintaining a balanced state. It’s a powerful connection that’s made me a firm believer in the value of regular check-ins. By tracking changes in my phase angle, I’ve gained insights that have nudged me towards proactive steps to keep my health on the upswing.
Now, let’s talk about how this all relates to cancer treatment. Monitoring phase angle is a powerful tool for healthcare providers. It helps them see how well treatments are working and how patients are bouncing back. By staying on top of this data, they can fine-tune treatments, giving patients the best shot at a full recovery. And for us patients, seeing that our treatments are paying off can be a game-changer, mentally and emotionally. It’s a big part of the healing process.
These scans, with their phase angle analysis, are like having a health coach in your corner, cheering you on with personalized insights. They paint a vivid picture of muscle mass, fat distribution, and hydration, all key players in the game of health. Armed with this knowledge, we can make smart choices about our diet, exercise, and lifestyle, leading to changes that stick and a healthier, happier life in the long run.
And let’s not forget the motivation that comes with it. When people see their phase angle improving, it’s like a high-five from their body, cheering them on to keep up the good work. Whether it’s tweaking their diet, getting more active, or finding ways to de-stress, the feedback from a phase angle analysis can be the nudge they need to make a change for the better.
By using phase angle analysis, we can make our health management more personal and effective. This will lead to a better quality of life for everyone.