For many, the term “REM sleep” is synonymous with the dream state, a surreal space where our most vivid and immersive dreams play out each night. But REM (rapid eye movement) sleep is more than just a portal to fantasy; it’s a vital phase in our sleep cycle, critical for processes such as memory consolidation, learning, and emotional regulation. In this comprehensive guide, we will explore the intricate web of factors that can either bolster or bog down your REM sleep, and how your daily activities and dietary choices may be affecting these important nighttime hours.
Understanding REM Sleep
Before we unravel the complex relationship between our lifestyle and REM sleep, it’s crucial to appreciate what REM sleep is and why it matters. REM sleep is one of four stages of a sleep cycle, which is patterned throughout the night. It usually begins about 90 minutes after you fall asleep, cycling through several times. During this phase, your eyes move rapidly from side to side behind closed eyelids, your brain waves mimic those of someone who is awake, and your breathing becomes faster and irregular.
This stage of sleep is where the majority of your dreams occur, and it’s also associated with processes that maintain our emotional health and flexibility. Disruptions to REM sleep have been linked to mood disorders such as depression and anxiety. Conversely, healthy REM periods are believed to help process the stress and emotional peaks of daily life, setting the stage for a rejuvenated and balanced wakefulness.
The Dance of Lifestyle Factors on REM Sleep
Our prevailing habits and routines have a dance with REM sleep that lasts all day. Each step, from the moment we wake until our heads hit the pillow, can affect the dance’s harmony and the quality of our REM experience.
The Rhythm of Routine
Maintaining a consistent sleep schedule is one of the golden rules for quality rest. Irregular sleep patterns can cause fragmentation of REM sleep, leading to a less restorative nighttime experience. For night owls and early birds alike, the key is to find a rhythm that allows for the required seven to nine hours of sleep each night, with an anchor time for waking and sleeping.
Stress and BEDtime Stories
Stress is a notorious saboteur of sound sleep, and this stands true for REM sleep. Chronic stress can reduce the overall amount of REM sleep, leading to undesirable emotional consequences such as increased irritability and difficulty coping with daily challenges. Cultivating a relaxing bedtime routine, free from the screens that emit blue light and the alerts that activate stress responses, can significantly aid in protecting your REM time.
Activity by Day, Rest by Night
Regular exercise can enhance the quality of all sleep stages, including REM. However, the timing is important. Intense workouts too close to bedtime can disrupt sleep. Experts suggest that moderate aerobic activity during the day can promote more deep and REM sleep when you hit the hay.

Ingesting Sleep: Dietary Choices and REM Sleep Correlations
The saying “you are what you eat” extends to “you sleep how you eat.” Our diet has a profound impact on sleep quality, and REM sleep is no exception.
Daytime Nutrition for Dreamy Nights
Foods rich in vitamins and minerals like magnesium, which is found in leafy greens, nuts, and whole grains, are associated with better sleep quality and can possibly enhance REM sleep. Meanwhile, a diet high in added sugars and saturated fats may decrease the amount of REM sleep you get each night while increasing your chances of waking up around with sugary cravings.
The Supper Affair
The last meal of the day should be a light affair, at least two to three hours before bedtime. A heavy, large meal can trigger indigestion, which can lead to disrupted REM sleep. Opting for smaller, nutritious suppers that contain substances like melatonin, magnesium and tryptophan can better prepare your body for a restful night. Foods such as cherries, dairy for those who can tolerate it, nuts, seeds and turkey, are all sources of these sleep-inducing nutrients.
The Drink Dilemma
Beverages, such as coffee and alcohol, are perhaps the most notorious culprits in the disruption of REM sleep. While it’s essential for many to have a morning cup to start the day, the half-life of caffeine means that even an afternoon coffee can linger in your system, potentially causing sleep disturbances, including a reduction in REM sleep. Alcohol, despite its initial sedative effects, can disrupt the overall organization of the sleep cycle and lead to lighter, less restful REM sleep later in the night.
Nurturing the Environment for REM Sleep
Creating a serene and sleep-conducive environment can provide a powerful boost to your REM experience. From the mattress you choose to the ambiance in your bedroom, every element of your sleep environment plays a part in the quality of your REM sleep.
The Bedtime Saga
A firm mattress and a supportive pillow are crucial for comfort and spinal alignment, which are key to relaxing enough to enter REM sleep. Old, worn-out mattresses and unsupportive pillows can cause discomfort and lead to frequent interruptions in your sleep cycle, interrupting your REM time.
The Atmosphere in Your REM Domain
The setup of your bedroom also matters. Is it dark enough? Cool enough? Free from distracting noises and sudden light intrusions? These environmental factors are the setting for a successful REM performance by your body, and they’re all within your control. Blackout curtains, ambient noise machines, and avoiding the blue light of electronic devices can all contribute to a more optimal sleep environment.

Balancing Act: Technology and Its Role in REM Sleep
In an age where screens are as ubiquitous as air, managing technology’s relationship with REM sleep is an ongoing balancing act. On one hand, technology can offer tremendous advancements in monitoring and improving sleep quality, but on the other, our constant connection to it can drive a wedge between us and the restful REM sleep we need.
The Monitoring Mania
Sleep-tracking apps and devices provide insights into the duration and quality of your various sleep stages, including REM. But like any tech, their usefulness depends on how you use them. Obsessively checking these trackers can lead to sleep anxiety, a condition where you become more worried and fixated on the notion that you’re not getting “enough” REM sleep, ironically making the situation worse.
The Digital Diet
The “blue light” emitted by smartphones, tablets, and laptops can suppress melatonin production, a hormone necessary for the onset of REM sleep. Establishing tech-free zones at least an hour before bedtime and utilizing blue-light filters on devices can mitigate its effects and support the quality of your REM time.

The Caffeinated Conundrum: Friends and Foes of REM Sleep
Caffeine is a staple in many daily routines, an essential wake-up call that precedes REM sleep by several hours. Its consumption can significantly affect your REM sleep, especially if you’re among the over 60% of Americans who admit they need coffee to start their day.
The Morning Cuppa
Caffeine’s stimulating effects on the nervous system can be felt within 15 minutes of consumption and can last between 6 to 8 hours. This means that you’re potentially still feeling the effects of your morning coffee by the time you’re ready to dream. Reducing or eliminating caffeine after noon ensures that the majority is out of your system by bedtime, thus decreasing the likelihood of REM sleep disruption.
The Afternoon Pick-Me-Up
While the afternoon lull may seem an appropriate time for a ‘pick-me-up’, a second or third cup of caffeine in the afternoon can delay the onset of REM sleep, leading to a decrease in the overall duration and density of REM segments during the night. Opting for a decaf or a non-caffeinated hot drink is a REM-friendly alternative that can help maintain the integrity of your sleep cycle.

Alcohol’s Journey in the Land of Z’s
Alcohol’s effects on sleep are complex and varied, but some trends are clear when it comes to REM sleep. Although it’s initially a sedative and can help you fall asleep faster, it can reduce the overall time spent in REM sleep.
The Nightcap Guide
Many turn to a nightcap to help them relax and fall asleep. While a small amount of alcohol might help with the former, it can lead to a decrease in deep sleep and an increase in lighter, non-REM stages. This means REM sleep is often more fragmented and concentrated in the second half of the night after alcohol levels in the blood have dropped.
The Ounce of Prevention
Minimizing alcohol consumption within a few hours of bedtime can help prevent the disruptions it causes to the quality and quantity of REM sleep. Opting for a non-alcoholic substitute can provide relaxation without the effects on your sleep cycle.

Cannabis and Counting Sheep
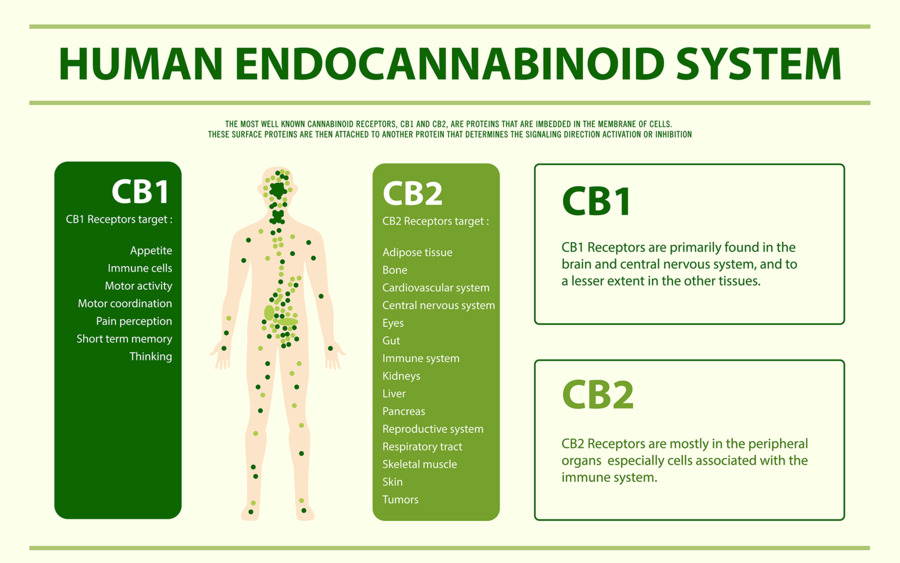
Research into the effects of THC (tetrahydrocannabinol) and CBD (cannabidiol) on REM (Rapid Eye Movement) sleep has yielded intriguing insights.
THC, the psychoactive component predominantly found in marijuana, has been observed to decrease the duration of REM sleep. Individuals consuming THC before bedtime may experience shorter REM sleep periods, which is the sleep phase associated with vivid dreams. This reduction in REM sleep might initially seem innocuous, particularly for those wishing to avoid nightmares, but long-term diminishment can affect the quality of rest and cognitive functions related to learning and memory consolidation that are believed to occur during this critical sleep stage.
On the other hand, CBD, a non-psychoactive compound, appears to have a more complex relationship with sleep. Some studies suggest that CBD might actually promote REM sleep stability, thereby potentially aiding those with REM Sleep Behavior Disorder (RBD), a condition characterized by physically acting out dreams. However, CBD’s effects can vary depending on dosage and individual response, highlighting the need for further research to fully understand its impact on sleep architecture.
For more articles on cannabis and sleep Click Here
Expert Tips and Advice for REM Sleep Optimization
Seeking insights from sleep specialists and experts can expand our understanding of how we can optimize REM sleep. These nuggets of wisdom can serve as beacons of knowledge in the vast sea of information on the subject.
The Doctor Is In
Sleep physicians often recommend the use of cognitive behavioural therapy for insomnia (CBT-I), a structured program that helps address the underlying causes of sleep problems. By examining and modifying behaviours and patterns related to sleep, such as caffeine use or bedtime routines, CBT-I has been shown to improve sleep quality and REM time.
Deep-Diving with a Dietician or Naturopath
Registered dieticians and Naturopathic Doctors can provide tailor-made dietary plans that focus on sleep-promoting foods, catering to individual nutrient needs and deficiencies. By including foods rich in magnesium, melatonin, and tryptophan, a dietician-guided diet can help support a healthy sleep cycle, including REM time.
For more naturopathic tips on better sleep Click Here
Hygiene with a Sleep Specialist
Consulting a sleep specialist or therapist can be a game-changer for those who consistently struggle with REM sleep. By working together to understand and address factors contributing to sleep disturbances, such as sleep apnea or other sleep disorders, expert care can offer significant improvements in REM sleep quality.
Conclusion: In the Lap of Awareness lies Quality REM Sleep
The road to enhanced REM sleep is paved with conscious choices and intentional actions. By developing a deeper awareness of the impact of our daily activities and dietary decisions on our sleep, we can foster an environment that supports the restorative power of our REM cycles.
A holistic approach that considers our unique needs, sensitivities, and challenges can yield the most sustainable results in our quest for sound sleep.
Call to Action: A Dream State of Being
Sleep is a barometer for health and well-being, and REM sleep is an integral part of that equation. Engaging in this discussion and learning more about the connection between our choices and our REM sleep empowers us to take control and achieve a dream state of being each and every night. Come join the quest for the ultimate sleep experience—your REM cycle and future self will thank you.
Those of you that read my articles regularly know that I am a WHOOP band wearer. Here is an article from WHOOP on how to optimize REM sleep








 I had used various natural sleep aids but needed a change as my current medication was producing some inconvenient side effects. After receiving my medical cannabis prescription I started using a balanced THC:CBD oil which improved my sleep latency and nighttime wakeup’s within a few days. Cannabinoid therapy is now one of my most recommended treatments for various types of insomnia as it is safe, inexpensive, fast acting and effective.
I had used various natural sleep aids but needed a change as my current medication was producing some inconvenient side effects. After receiving my medical cannabis prescription I started using a balanced THC:CBD oil which improved my sleep latency and nighttime wakeup’s within a few days. Cannabinoid therapy is now one of my most recommended treatments for various types of insomnia as it is safe, inexpensive, fast acting and effective. Many chronic diseases that have been linked to disruption in the endocannabinoid system (Fibromyalgia, Migraine, Inflammatory Bowel Disorder) have a sleep disruption comorbidity. This sleep disruption can usually be helped with a prescription of cannabinoids such as CBD. It is certainly plausible and empirical evidence supports the theory that patients with sleep disorders have endocannabinoid disruption. Therefore, phystocannabinoids like CBD can be helpful to restore endocannabinoid tone and subsequently better sleep.
Many chronic diseases that have been linked to disruption in the endocannabinoid system (Fibromyalgia, Migraine, Inflammatory Bowel Disorder) have a sleep disruption comorbidity. This sleep disruption can usually be helped with a prescription of cannabinoids such as CBD. It is certainly plausible and empirical evidence supports the theory that patients with sleep disorders have endocannabinoid disruption. Therefore, phystocannabinoids like CBD can be helpful to restore endocannabinoid tone and subsequently better sleep.