A concussion is a mild traumatic brain injury caused by a bump, jolt, or blow to the head. If you’ve been diagnosed with a concussion, you may be wondering what you should do next. This blog post will provide some helpful tips on how to manage your recovery process.
Allow Your Brain Time to Heal
First and foremost, it’s important to give your brain the time it needs to heal after sustaining a concussion. It can take anywhere from several days to several months for someone with a concussion to feel completely better. In general, most people experience symptoms for up to three weeks following the injury. During this time, it’s important that you rest both mentally and physically in order for your symptoms to improve.
Recent research has shown that the amount of rest required after a concussion to help a person heal and recover is more than what was previously thought. In order for an individual to experience the most beneficial results, it is suggested that they take at least 24 hours of rest following a concussion. This includes not only avoiding physical activity, but also limiting activities that require mental exertion and concentration, such as watching television or playing video games. It is important to note that this initial period of rest should be followed by gradually increasing activity as symptoms improve, with sufficient breaks built in throughout the day.
Additionally, studies suggest that adolescents need between 10-14 days of rest in order to achieve full recovery from a concussion. This extended period of rest could include reduced physical or cognitive activities and even temporarily stopping school or work obligations if necessary.
Ultimately, the amount of rest required after suffering a concussion will vary depending on each individual’s specific needs and symptoms. However, research has demonstrated that taking at least 24 hours of complete rest initially and then gradually increasing activity levels as symptoms improve can be an effective way for individuals to recover faster and live healthier lives.

Diet after concussion
Eating a diet that is rich in essential nutrients and vitamins can be an important part of recovery after concussion. Eating plenty of fruits, vegetables, and lean protein can help support brain health and provide the necessary nutrients to aid in neurocognitive functioning after a concussion. Studies have shown that consuming foods with omega-3 fatty acids, such as fish and nuts, may help reduce the risk of long-term cognitive impairment associated with concussions (Hoffman et al., 2015).
In addition, research suggests that eating large amounts of antioxidant-rich foods like berries, spinach, and kale can help to protect against inflammation caused by traumatic brain injuries (TBIs) (Fotuhi et al., 2016).
Furthermore, having adequate levels of vitamin D has been linked to improved outcome from TBIs (Xiao et al., 2018). Therefore it is important for individuals who have experienced concussions to consume a balanced diet that includes several servings of fruits and vegetables daily along with lean protein sources like fish or poultry. Additionally, eating smaller meals throughout the day rather than three large meals may also improve cognitive functioning after a concussion (Cantu & Nowinski, 2007).
Finally, drinking adequate amounts of water throughout the day is essential for maintaining proper hydration which helps support healing processes in the brain following traumatic injury. With these considerations in mind, dietary changes can be an invaluable tool in supporting recovery from concussion.

Exercise following concussion
Exercise can be an incredibly helpful tool for recovery after concussion. Physiotherapy or physical therapy (PT) is a common way to help individuals recover from concussions, and exercise plays an important role in this process.
Exercise has been shown to reduce symptoms of concussion such as headaches, dizziness, and difficulty concentrating (Giza et al., 2020). It can also improve overall balance and coordination, which are both key components of post-concussion recovery (Peterson & Pfister, 2020).
Additionally, exercise can help reduce anxiety and depression after concussion by providing structure and routine to each day (Roche et al., 2019). Studies have found that aerobic exercise is especially beneficial in post-concussion recovery. Aerobic exercises such as cycling or walking can increase blood flow to the brain and may also stimulate neuroplasticity in the brain cells that were affected by the concussion (Cantero et al., 2017).
By providing a safe environment with gradual increases in intensity over time, PTs are skilled at helping individuals develop an exercise plan tailored to their needs that will support their recovery. Thus, when used properly under professional guidance, exercise can be an effective tool for promoting healing after a concussion.
Sleep
Getting enough quality sleep after a concussion is one of the most important things to aid in recovery. When one suffers from head trauma, their body needs more time to heal and rest than it usually does. Without adequate rest, the healing process can be significantly delayed or slowed. Quality sleep not only allows for healing to occur but also helps individuals maintain balance, improve decision-making, and promotes physical and mental wellbeing (Liu & Ledden, 2020).
Individuals with concussions should get between seven and nine hours of quality sleep each night as recommended by the National Sleep Foundation (NSF, 2021). This amount of restful sleep may vary depending on individual circumstances.
Strategies such as avoiding caffeine after lunchtime, limiting exposure to bright screens before bedtime and establishing a regular bedtime routine can also help support recovery from concussion-related symptoms (Callaghan et al., 2019). Creating a comfortable sleeping environment free from noise, light and other distractions is important for allowing the body’s natural healing processes to occur during sleep (Freeman et al., 2017).
In addition to increasing restful sleep, individuals with concussions may benefit from engaging in activities such as yoga or mindfulness exercises that are known to reduce stress levels which can improve overall health including mental clarity (Kim et al., 2018). These activities paired with ample amounts of quality sleep may help speed up recovery time while promoting balance, improved moods and functioning following a concussion.

Supplements for concussion recovery
There are a number of dietary supplements that have been shown to assist healing after sustaining a concussion.
Omega-3
One key supplement is omega-3 fatty acids, which have been found to reduce post-concussion symptoms such as headaches and confusion, as well as helping to improve cognitive functions like memory and focus.
Studies have found that Omega-3 fatty acids can reduce inflammation of the brain, which is a primary factor in concussions and other types of traumatic brain injuries. It has also been demonstrated that Omega-3s help protect brain cells from damage caused by free radicals and oxidative stress, which are both associated with at least some forms of head trauma.
Furthermore, research has suggested that Omega-3s might help improve cognitive function and motor coordination following a concussion. In particular, studies have pointed to the potential for Omega-3s to increase the speed at which athletes return to play following a concussion. For example, one study conducted on collegiate football players found that those who took daily doses of fish oil for 2 weeks before their season had significantly less downtime due to post-concussive symptoms compared to those who did not take supplementation (Mazzuca et al., 2018).
Another randomized controlled trial showed that daily consumption of 1 gram per day of omega-3s was associated with improved memory performance post injury (Dang et al., 2016).
Collectively, these findings suggest that Omega-3 supplementation may be an effective tool for supporting recovery after concussion.

Vitamin D
A growing body of evidence indicates that supplementing with vitamin D can help to reduce the severity and duration of symptoms associated with a concussion, as well as help to improve cognitive functioning. For example, a study in the American Journal of Clinical Nutrition found that participants who supplemented with 4,000 IU of vitamin D per day for 12 weeks reported significant improvements in balance, reaction time, and tactile sensitivity compared to those who did not receive supplementation.
Additionally, a review published in the journal Sports Medicine found that supplementing with vitamin D may reduce the amount of time it takes for an individual to return to their baseline performance after suffering from a concussion. This is likely due to its neuroprotective effects and ability to reduce inflammation.
Vitamin D also appears to have beneficial effects on depression-like symptoms which can occur after a concussion. A study published in BioMed Research International found that among individuals who had suffered minor head injuries or mild TBIs, those who supplemented with vitamin D saw greater improvement in depressive symptoms than those who did not receive supplementation. Overall, these findings suggest that supplementing with vitamin D may be a beneficial adjunct treatment for aiding recovery after concussion or other mild brain injuries.
Magnesium
Magnesium supplementation has been found to be beneficial in supporting recovery after concussion. A recent systematic review of studies published in the American Journal of Medicine concluded that magnesium supplements may reduce the severity, duration, and frequency of post-concussion symptoms such as headaches, sleep disturbances, dizziness, and cognitive impairments.
In addition to reducing symptoms following a concussion, magnesium supplementation has also been shown to aid in the repair of neuronal damage caused by the trauma. For example, a study published in The Neuroscientist journal showed that magnesium was able to attenuate neuronal damage by increasing protective proteins and reducing glutamate levels in rats with traumatic brain injury (TBI).
Furthermore, a study conducted on college football players revealed that those who received magnesium supplements reported fewer concussions over a three year period than those who did not receive supplementation. This suggests that magnesium may provide some protection against concussions by increasing brain resilience and aiding in recovery after an event occurs.
While more research needs to be done in order to gain further insights into how magnesium affects the recovery process following a concussion, current evidence suggests that it is a safe and effective way to help support recovery after such an injury.
Cannabidiol
CBD has been found to be a valuable supplement for those who have sustained a concussion. Studies have shown that CBD can help reduce inflammation, which can occur after a traumatic brain injury (TBI). It can help stabilize the post-injury neurochemistry of the brain, which is often affected due to a concussion. People who use CBD after sustaining a concussion often report feeling more alert and motivated, as well as having better concentration and short-term memory. CBD is also known to decrease anxiety and depression, two common side effects of TBIs.
CBD can also help to reduce headaches and improve sleep quality, both of which are important for healing from a concussion. Furthermore, some studies suggest that CBD may even protect against future cognitive decline by preserving brain cells and protecting them from damage caused by free radicals. All in all, taking CBD following a concussion could make the healing process easier and more comfortable for those who have experienced head trauma. As with all supplements it is important to consult with your healthcare practitioner prior to use in order to know proper dosage and common side affects and interactions.

Vitamin B12
Vitamin B12 supplementation can be an effective tool for recovery after concussion, as evidence suggests that B12 deficiency may contribute to post-concussion syndrome. One study found that patients with chronic post-concussion syndrome were more likely to have lower serum B12 levels, suggesting a potential link between Vitamin B12 deficiency and the condition (Al Abed et al., 2018). B12 supplementation has also been suggested as a potential treatment for post-concussion headaches due to its anti-inflammatory properties (Lakhani et al., 2020).
Additionally, Vitamin B12 has been shown to support cognitive function by aiding in the biosynthesis of neurotransmitters, which are essential for proper brain functioning (Matthews et al., 2016).
Zinc
Zinc is an essential mineral for human health, and supplementation with zinc has been linked to faster recovery times from concussion. Evidence from a study published in the Journal of Neurotrauma suggests that zinc may improve recovery time following a concussion. In their study, researchers found that administration of zinc sulfate within 24 hours after the initial diagnosis of concussion significantly improved recovery outcomes for patients.
Another study in the journal Nutrients showed that taking high doses of zinc was associated with better cognitive performance following a mild traumatic brain injury (mTBI). This is likely due to the fact that zinc plays an important role in the structural integrity of synapses and neurons, as well as helping to reduce inflammation in the brain which can occur after concussions. Taken together, these studies suggest that supplementing with zinc can be beneficial for those who suffer from a concussion and should be strongly considered for those looking to enhance their recovery times.
Probiotics
The use of probiotic supplementation to support recovery from concussions is gaining increased recognition in the medical community. Research conducted on this topic has consistently demonstrated that probiotics may be beneficial for those recovering from mild-to-moderate traumatic brain injury (TBI).
A study published in 2017 showed that daily consumption of a probiotic supplement containing both Lactobacilli and Bifidobacteria, resulted in an improvement in cognitive functioning, including attention and verbal memory, as well as enhanced emotional regulation up to 6 months after TBI. This finding offers potential new treatment strategies for those recovery from concussion-related symptoms.
Other studies have also indicated that probiotics may be useful for patients suffering from post-concussive syndrome (PCS). In a randomized controlled trial conducted in 2018, researchers found that participants who took a multispecies probiotic supplement reported fewer PCS symptoms one month following their treatment than did those who received the placebo. Furthermore, another study showed that taking a probiotic supplement daily could reduce levels of systemic inflammation, which has been linked to longer periods of recovery time following a concussion.
Overall, there is evidence to suggest that probiotics can play an important role in supporting concussion recovery by providing neuroprotection and promoting overall health. Probiotics have been identified as having neuroprotective effects due to their ability to promote gut homeostasis and modulate neuroinflammatory processes which can help improve cognition and reduce inflammation.
While further research is needed to determine the exact mechanisms by which probiotics might support recovery following concussion, current findings suggest that this type of supplementation may be an effective adjunctive treatment option.

Curcumin
Curcumin supplementation may have a beneficial effect on recovery from concussion. This is because curcumin is a powerful antioxidant that scavenges oxidative stress and inflammation, both of which can contribute to the progression of post-concussion syndrome (PCS) symptoms. A 2019 study published in the journal Brain Impairment found that curcumin supplementation significantly reduced PCS symptoms in patients with mild traumatic brain injury when compared to placebo. The study concluded that curcumin has potential as an effective supplement for reducing PCS symptoms.
Additionally, another study published in 2020 in the European Journal of Nutrition found that curcumin improves cognitive function after experiencing a concussion due to its anti-inflammatory properties. Participants of this study experienced improved memory and attention following supplementation with curcumin over the course of six weeks.
Furthermore, another 2020 study published in Brain Injury showed that curcumin supplementation may protect against microglial activation, which is one of the leading causes of inflammation after a concussion. This suggests that by supplementing with curcumin, individuals may be able to reduce their risk for developing neuroinflammation after sustaining a concussion.
Glutamine
Glutamine supplementation may be a valuable tool to support recovery after concussion. Research has shown that glutamine supplementation can reduce cerebral edema and improve neurovascular autoregulation after concussion, as well as promote repair of damaged neurons and axons. Studies have also suggested that glutamine supplementation can reduce post-concussion symptoms such as headache, dizziness, confusion, difficulty concentrating, memory loss and fatigue.
One study reported that patients with mild traumatic brain injury who received glutamine supplements experienced faster resolution of their symptoms compared to those who did not receive supplements. Another study found that participants with moderate-to-severe traumatic brain injury who received glutamine supplements had improved cognitive performance on tests measuring attention span and working memory. Thus, glutamine supplementation can be beneficial for recovery from concussion by helping to reduce symptoms associated with injury and aiding in neurological repair processes.
Carnitine
Studies have demonstrated that the administration of the amino acid L-carnitine, in combination with traditional physical and cognitive therapy, can lead to faster and more complete recovery from concussion.
Carnitine helps to maintain the brain’s energy balance, as it helps transport fatty acids across mitochondrial membranes for energy production. This process helps support healthy neural pathways, which can help reduce the symptoms of concussion and improve overall recovery time.
Additionally, carnitine works to protect neurons from oxidative damage by stimulating antioxidant activities and increasing glutathione levels in the brain. Observational studies suggest that carnitine supplementation may also alleviate some of the long term consequences associated with concussion such as decreased concentration and memory issues.
CoQ10
Finally, Coenzyme Q10 has been found to protect brain cells from free radical damage caused by a traumatic event like a concussion, helping to speed up the healing process.
CoQ10 supplementation has been studied as a potential tool to support recovery after concussion. In one study, patients with mild traumatic brain injury were given CoQ10 for 8 weeks and demonstrated improved neurological symptoms compared to the placebo group. Specifically, the CoQ10 group reported reduced headache frequency and intensity, increased cognitive performance on a standard battery of tests, and overall reduction in disability.
In another study, patients with acute mild traumatic brain injury were supplemented with CoQ10 for 8 weeks. Participants reported statistically significant improvements in quality of life, cognition, and alertness when compared to those who received a placebo. Additionally, MRI scans performed on the subjects revealed less white matter lesions in those who had been provided CoQ10 as opposed to the control group.
CoQ10 supplementation can be used to support recovery after concussion by improving clinical scores related to cognition and disability while also helping reduce oxidative stress and inflammation associated with MTBI pathology.
All these supplements should be taken under the guidance of a healthcare provider in order to maximize their effectiveness in treating and healing a concussion.
Be Mindful of Your Symptoms
It’s important that you monitor your symptoms closely after sustaining a concussion so that if they get worse, you can seek medical help right away. Common signs and symptoms include headaches, dizziness, nausea/vomiting, sensitivity to light and noise, difficulty concentrating or remembering things, feeling tired all the time, blurred vision or double vision, slurred speech, and irritability/mood changes such as depression or anxiety. If any of these symptoms persist beyond three weeks following the injury or become severe enough interfere with daily life activities (e.g., work/school), you should contact your healthcare provider for further evaluation and treatment if necessary.

Conclusion
Recovering from a concussion can take anywhere from several days to several months. Everyone heals differently depending on individual circumstances such as age, medical history etc., so it’s important that you talk with your healthcare provider about what will be best for managing your particular situation going forward. By allowing yourself time to heal mentally and physically while being mindful of any changes in symptomotology throughout the recovery process and following all instructions provided by your healthcare provider accordingly will help ensure an optimal recovery outcome long-term!
Multiple sclerosis is a debilitating neurological disorder that can often leave patients feeling hopeless and alone. But there is hope! In this blog post, we will explore nine natural treatments for multiple sclerosis that have helped my Toronto patients alleviate some of the symptoms associated with the disease.
1. Acupuncture
Acupuncture is a traditional Chinese medicine technique that involves inserting thin needles into the skin at specific points on the body. It is believed that this helps to clear energy blockages and promote balance and healing within the body. There is some evidence to suggest that acupuncture may be effective in treating symptoms of multiple sclerosis, such as fatigue, pain, spasticity, and bladder problems.
2. Herbal Medicine
There are many different herbs that have been traditionally used to treat various ailments, including multiple sclerosis. Some of the most common herbs used for MS include ginger, ginkgo biloba, turmeric, milk thistle, lions mane and green tea. These herbs can be taken in pill form or brewed into a tea. It is important to talk to a Naturopathic Doctor or qualified herbal practitioner before starting any herbal treatment regimen, as some herbs can interact with medications you may be taking for your MS.
3. Dietary Changes
Making some simple dietary changes can also help improve symptoms of MS. One study showed that following a Mediterranean diet—which includes lots of fresh fruits and vegetables, whole grains, fish, and olive oil—may help reduce inflammation and slow the progression of MS. Other helpful dietary changes include avoiding processed foods and food allergies, getting enough vitamin D, and drinking plenty of water.
Food sensitivity testing can help to identify gluten sensitivity and other food sensitivities in people with MS and other autoimmune diseases. The most common type of food sensitivity test is an Elimination Diet, in which potential triggering foods are eliminated from the diet for a period of time and then reintroduced one at a time to see if symptoms occur. However, Elimination Diets can be difficult to stick to and can take months or even years to complete. Another option is an IgG Food Sensitivity Test, which measures levels of immunoglobulin G (IgG) antibodies in the blood.
Antibodies are produced by the immune system in response to perceived threats, such as bacteria or viruses. However, in people with food sensitivities, the immune system overreacts to harmless proteins found in certain foods, producing excessive amounts of IgG antibodies. IgG Food Sensitivity Tests can be helpful in identifying food sensitivities because they can measure levels of IgG antibodies specific to each individual food protein. This allows for a more targeted Elimination Diet and can speed up the diagnosis process. If you think you might have a food sensitivity, you can book an appointment for testing.
4. Exercise
Exercise is important for everyone, but it is especially crucial for those with MS. Regular physical activity can help reduce fatigue, improve mobility and coordination, ease depression and anxiety, promote better sleep, and boost overall fitness and well-being. Even if you are not able to do strenuous exercise due to your symptoms, there are still many low-impact activities you can do to get moving and feeling better.
5. Stress Reduction Techniques
Stress is a well-known trigger for multiple sclerosis (MS) flare-ups. Managing stress is therefore an important part of MS treatment. Stress management techniques such as relaxation therapy and yoga can be helpful, but some patients may also benefit from taking adaptogens. Adaptogens are a class of natural substances that help the body to adapt to stress by reducing the production of stress hormones. They have been used for centuries in traditional Chinese and Indian medicine, and are now gaining popularity as a natural treatment for stress and anxiety. Some common adaptogens include ashwagandha, holy basil, and ginseng. If you are interested in trying adaptogens, talk to your Naturopathic doctor first to discuss whether they are right for you.
6. Vitamin D
Vitamin D is an important nutrient that helps the body absorb calcium. It’s found naturally in very few foods, so most people get it from exposure to sunlight. Vitamin D is also available in supplement form. Some studies suggest that vitamin D may play a role in helping to prevent or treat MS. If you think you might be deficient in vitamin D, book an appointment with us for vitamin D testing or talk to your doctor.
Sometimes supplementation is ineffective or can take too long to bring up severely deficient vitamin D levels. I offer these patients the option of a high potency vitamin D injection that will bring levels up very quickly.
7. Mitochondrial Support
Mitochondrial support using resveratrol, alpha lipoic acid, coenzyme Q10 and NAD boosters is a promising new treatment for patients with multiple sclerosis. Mitochondria are the powerhouses of the cell, and they are responsible for producing energy. In patients with multiple sclerosis, the mitochondria are not working properly, and this can lead to fatigue and other symptoms. Resveratrol, alpha lipoic acid, coenzyme Q10 and NAD boosters help to support the mitochondria and improve their function. In a small study of patients with multiple sclerosis, those who received mitochondrial support had less fatigue and improved quality of life.
8. Hormones
Hormones play an important role in the human body, regulating everything from metabolism and mood to reproduction and energy levels. When hormones are out of balance, it can lead to a host of problems. For patients with multiple sclerosis (MS), hormone imbalances can cause fatigue, weight gain, depression, and loss of libido. Hormone testing can help to identify imbalances and allow for tailored treatment plans that use bio identical hormone replacement therapy to restore balance. By addressing hormone imbalances, patients with MS can improve their quality of life and potentially reduce their risk of disease progression.
9. Cannabinoids
Recently, cannabinoids have emerged as a potential therapy for MS. Cannabinoids are compounds found in the cannabis plant, and they have been shown to have anti-inflammatory and neuroprotective effects. In animal studies, cannabinoids have been shown to reduce inflammation and nerve damage in models of MS. In small clinical trials, cannabinoids have been shown to improve symptom control in patients with MS. These promising results have led to the development of several cannabinoid-based medications for MS. Dr. Shawn Meirovici N.D. is experienced cannabis educator in Toronto, Ontario. Dr. Shawn can help patients decide if cannabis therapy would be a good addition to their treatment plan.
Conclusion:
If you are living with multiple sclerosis (MS), know that you are not alone—there are millions of other people around the world dealing with this disease every day. And while there is no cure for MS at this time, there are many different treatments that can help alleviate some of the symptoms associated with the disease. In this blog post, we explored nine natural treatments for MS—acupuncture , herbal medicine , dietary changes , exercise , stress reduction techniques, vitamin D, mitochondrial support, hormone balancing and cannabinoid therapy. Make an appointment with us or talk to your doctor about which treatments might be right for you.
Cannabinoid therapy for sleep
I have noticed consistently good results using cannabinoids for sleep disorders. I am often asked what are the top indications for cannabis therapy in my practice and insomnia would always be in the top three.
I first started to gain an interest in cannabis and cannabinoids back in 2015. One of the most common reasons that my patients were using cannabis was for various types of insomnia. Most of these patients were having very good results. That really peaked my interest because I too suffered from insomnia for a large part of my life.
 I had used various natural sleep aids but needed a change as my current medication was producing some inconvenient side effects. After receiving my medical cannabis prescription I started using a balanced THC:CBD oil which improved my sleep latency and nighttime wakeup’s within a few days. Cannabinoid therapy is now one of my most recommended treatments for various types of insomnia as it is safe, inexpensive, fast acting and effective.
I had used various natural sleep aids but needed a change as my current medication was producing some inconvenient side effects. After receiving my medical cannabis prescription I started using a balanced THC:CBD oil which improved my sleep latency and nighttime wakeup’s within a few days. Cannabinoid therapy is now one of my most recommended treatments for various types of insomnia as it is safe, inexpensive, fast acting and effective.
Cannabis can have calming or stimulating effects depending on the preparation, dose and mode of administration. I really wanted to find out what made cannabis effective for sleep and what would be the optimal way to use it for sleep. My research pointed towards a few mechanisms through which cannabinoids likely have sleep promoting effects: GABA, Serotonin and Endocannabinoid modulation.
GABA
GABA is an inhibitory neurotransmitter that generally promotes a relaxation response in the central and peripheral nervous system. It is well established that activation of GABA receptors favours sleep and many pharmaceutical drug classes, including benzodiazepines, act on GABA receptors.
Both animal and human studies have demonstrated that cannabidiol (CBD) has a modulatory effect on GABA activity. CBD can both increase and decrease GABA activity depending on neurotransmitter activity levels (if there’s too little it increases, if there is too much it decreases). This makes CBD useful for sleep disorders resulting from too little GABA activity (think of the overactive brain) without the addictive potential of GABA stimulating pharmaceutical preparations.
Serotonin
Serotonin is a neurotransmitter that is involved in mood and sleep/wake responses. Many antidepressant medications specifically target serotonin activity. Research from the early 2000’s by Bambico et al demonstrated that cannabinoid receptor agonists (things that stimulate cannabinoid receptors) have the ability to modulate serotonin activity. Low doses seemingly to raise serotonin activity while high doses have little effect.
Both endogenous cannabinoids (cannabinoids we make ourselves) and phytocannabinoids (THC, CBD etc..) seem to have the ability to modulate serotonin activity via stimulation of our cannabinoid receptors. This may explain some of the physiology involved in the sleep promotion and anti-anxiety effects of cannabis preparations. CBD seems to be particularly useful through its interplay with our endocannabinoid system.
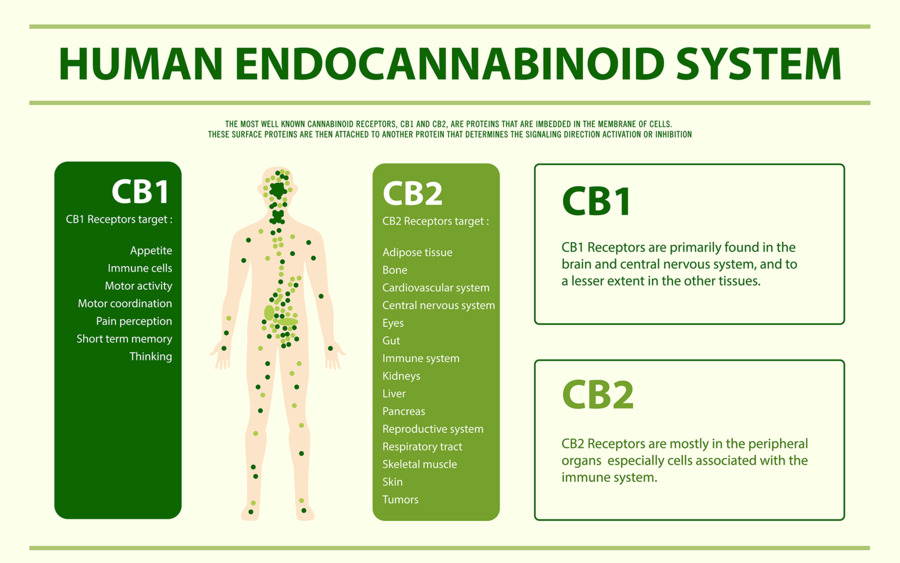
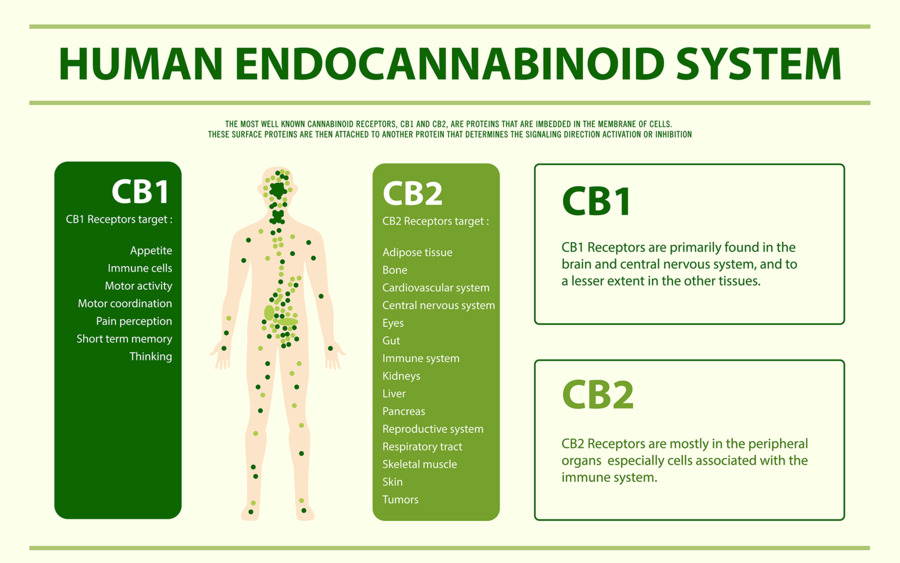
The Endocannabinoid System
All species, with the exception of insects, have an endocannabinoid system. The endocannabinoid system is our bodies harm reduction system, keeping chemical and electrical singling in balance. Overall, stimulation of the endocannabinoid system has a calming effect and a known modulator of our sleep/wake cycle.
 Many chronic diseases that have been linked to disruption in the endocannabinoid system (Fibromyalgia, Migraine, Inflammatory Bowel Disorder) have a sleep disruption comorbidity. This sleep disruption can usually be helped with a prescription of cannabinoids such as CBD. It is certainly plausible and empirical evidence supports the theory that patients with sleep disorders have endocannabinoid disruption. Therefore, phystocannabinoids like CBD can be helpful to restore endocannabinoid tone and subsequently better sleep.
Many chronic diseases that have been linked to disruption in the endocannabinoid system (Fibromyalgia, Migraine, Inflammatory Bowel Disorder) have a sleep disruption comorbidity. This sleep disruption can usually be helped with a prescription of cannabinoids such as CBD. It is certainly plausible and empirical evidence supports the theory that patients with sleep disorders have endocannabinoid disruption. Therefore, phystocannabinoids like CBD can be helpful to restore endocannabinoid tone and subsequently better sleep.
Dosing Considerations
Cannabis is a unique medicine as it cannot be prescribed based on age and weight. Everyone has an individual response to cannabinoids due to the fact that everyone has unique endocannabinoid tone and metabolism.
Cannabinoids like CBD and THC can interact with particular medications and preexisting conditions. Some preparations of cannabis are very different in their effect and duration. Smoked cannabis has a very fast acting effect but a short duration. Edible cannabis can have a slow onset of effect but last for a long time.
Therefore it is highly recommended to have a healthcare professional knowledgeable in cannabinoid therapy work with you for the initial stages of treatment. This will ensure a safe and effective dosing strategy with minimal chance for adverse effects. With that being said cannabis is a very safe medication and when prescribed correctly can make a significant difference in those suffering from sleep disorders. Check out the Cannabis Therapy page for more information.
References
Pretzsch CM, Freyberg J, Voinescu B, Lythgoe D, Horder J, Mendez MA, Wichers R, Ajram L, Ivin G, Heasman M, Edden RAE, Williams S, Murphy DGM, Daly E, McAlonan GM. Effects of cannabidiol on brain excitation and inhibition systems; a randomised placebo-controlled single dose trial during magnetic resonance spectroscopy in adults with and without autism spectrum disorder. Neuropsychopharmacology. 2019 Jul;44(8):1398-1405. doi: 10.1038/s41386-019-0333-8. Epub 2019 Feb 6. PMID: 30758329; PMCID: PMC6784992. Gottesmann C. GABA mechanisms and sleep. Neuroscience. 2002;111(2):231-9. doi: 10.1016/s0306-4522(02)00034-9. PMID: 11983310. Moreira FA. Serotonin, the prefrontal cortex, and the antidepressant-like effect of cannabinoids. J Neurosci. 2007 Dec 5;27(49):13369-70. doi: 10.1523/JNEUROSCI.4867-07.2007. PMID: 18057193; PMCID: PMC6673093.
What is Long Covid?
Long Covid is defined as symptoms that present 12 weeks after infection and that persist for at least 8 weeks. The most common symptoms being: Fatigue, Shortness of Breath and Cognitive Dysfunction. There will be an estimated 150 million cases of Long Covid cases worldwide as of 2022. Long Covid has the potential to significantly impact the lives of a large portion of the population making day to day activities difficult or near impossible. Although there are ways to reduce the risk factors in developing long covid, there aren’t many proven conventional medications to treat Long Covid once symptoms set in.
We now know that viral fragments, lingering spike protein and persistent inflammation are all likely features of Long Covid. This chronic state of immune activation leads to heart and blood vessel abnormalities, lung impairment, neurological injury and autoimmunity. Luckily, functional medicine practitioners have been at the forefront in developing protocols that work to resolve the aftermath of COVID-19 infection.
Mitochondrial Dysfunction
There is evidence of mitochondrial dysfunction in Long Covid cases as seen through disruption in fatty acid oxidation and altered lactate production. This would also partially explain the chronic fatigue of Long Covid. Functional medicine has a long history of developing protocols to address mitochondrial dysfunction. Many of the compounds used have been showing promise in treating Long Covid. For example, there is evidence of reduced levels of Coenzyme Q10 in COVID-19 infection. CoQ10 is an important compound in mitochondrial function and energy production. Supplementing with this compound along with other mitochondrial supportive nutrients (Niacin, N-Acetyl Cysteine, Alpha Lipoic Acid) have been helpful in treating Long COVID associated fatigue.
Chronic Inflammation
We also know that there is a wealth of data to suggest high levels of inflammatory markers in Long Covid sufferers. Conventionally, steroids such as prednisone have been used to effectively treat Long Covid symptoms. However, steroids can not be used indefinitely as there are significant side effects associated with long term usage. In Naturopathic and Functional Medicine we have evidence of a number of naturally derived compounds that work to treat Long Covid associated inflammation including: Curcumin, Resveratrol, Cannabinoids, Luteolin, Omega 3, and Black Cumin.
Immune System Abnormalities
We also know that there is immune system dysfunction in Long Covid as evidenced in abnormal T-cell behaviour. One of the most important compounds regulating immune function is vitamin D. There is strong evidence that having adequate vitamin D status prior to Covid infection is protective toward Long Covid and giving large doses of vitamin D to both active Covid-19 cases and Long Covid sufferers can be therapeutic.
Gastrointestinal Symptoms
Long Covid cases also seem to have a higher incidence of prolonged gastrointestinal symptoms and intestinal dysbiosis with organisms that increase inflammation. One of the best ways to treat intestinal inflammation is by promoting the growth of intestinal organisms that produce the short chain fatty acid Butyrate. Food that is high in fibre typically help to promote beneficial species of intestinal organisms. Oats, Apples, Onions, Asparagus, Broccoli, Whole grains, underripe bananas, Legumes, and Berries are some excellent foods shown to promote butyrate production.
Cannabinoids
Cannabinoids, and more specifically cannabidiol (CBD) has been shown to have some interesting mechanisms in the treatment of Long Covid. Strains of cannabis containing high levels of CBD have been shown to block spike protein from entering the cell (via ACE-2 receptors), modulate ACE-2 receptor density on cell surfaces (less doors of COVID to enter) and reduce inflammation. Therefore cannabinoids are very exciting compounds currently being investigated for use in Long Covid therapy.
Conclusions
Long Covid is a multifaceted chronic disease with effects on various physiological systems. Drugs with a narrow therapeutic scope are not going to be as effective as complex compounds that effect multiple physiological processes at the same time. This type of therapeutic synergy is a hallmark of naturally derived medicines and therefore functional medicine is going to play a pivotal role in dealing with this prevalent and highly complex disease state. In my Toronto practice I have had several cases of long covid that only began to resolve once a functional medicine protocol was put into place. So if you know someone who is suffering from Long Covid I recommend connecting them with a local Naturopathic Doctor or Functional Medicine Practitioner.
The mind body connection
The mind and body are closely connected through thousands of chemical messengers. When we have a mental experience the brain sets off a cascade of neurotransmitters and hormones that affects our body. For instance when we experience joy, our body produces the hormone oxytocin. Oxytocin reduces blood pressure, stress hormone, anxiety and promotes growth and healing. Conversely, when we experience an emotion like sadness this can raise stress hormone, increasing blood pressure and eliciting negative effects on the immune system. Psychotherapy can therefore have a big impact on the health of our body by modifying mental outlook and thus inducing positive chemical messengers to the rest our body. An example is cognitive behavioural therapy, which has well documented success in the treatment of depression, anxiety and stress. https://pubmed.ncbi.nlm.nih.gov/ 31004323/
We can also treat conditions of the mind through our body. In pharmaceutical medicine, drugs like anti-depressants can block the breakdown of the neurotransmitter serotonin. Serotonin is involved in mood and therefore in some individuals boosting serotonin activity can improve mood and decrease anxiety. However, some short falls of pharmaceutical medicine is that it can often cause unwanted side effects and have a narrow therapeutic range; meaning that too little may have no effect and too much can be deadly. There are also issues with dependancy and addiction.
On the other hand nutritional and herbal supplementation can be an effective treatment for depression, stress and anxiety without the same safety concerns as drugs.
Supplementation for depression
Depression is both a physical and emotional condition. We know that depression can impact the reproductive system, immune system and our nervous system. Nutritional deficiencies can arise as a result of long standing depression and can be a precursor in the development of a depressive condition. Deficiencies in vitamin B12, vitamin D and protein are associated with depression. https://pubmed.ncbi.nlm.nih.gov/ 23377209/ In my Toronto clinic we can identify and correct nutritional deficiencies and make a big impact on depressive symptoms.
There is also a lot to be said about the impact of chronic inflammation on brain and mental health. Research has shown that chronic inflammation can increase susceptibility to depression. https:// pubmed.ncbi.nlm.nih.gov/32553197/ At the Toronto clinic we treat inflammation using supplements such as curcumin, omega-3 fatty acids and cannabidiol (CBD). These supplements can improve depressive symptoms through modulation of inflammation.
Furthermore many natural health products like CBD can also impact neurotransmitters (brain messenger chemicals) directly associated with depression. Through the interaction of cannabinoid receptors, 5-HT1A (involved in serotonin regulation) and neurogenesis factors CBD can act similarly to an anti-depressant medication but with less potential for adverse effects. At the Toronto clinic I offer cannabis education and counselling when cannabinoids would benefit a patients condition.
Supplementation for Anxiety
Anxiety disorders are the most common mental illness in the United States effecting close to 20% of the population every year. While genetics play a significant role in the development of an anxiety disorder, biological and environmental factors are pivotal as well. We know that there are often disruptions in serotonin and dopamine, cortisol and adrenaline in anxiety syndromes. A common class of drugs used in the treatment of anxiety are the benzodiazepines (Xanax, Valium, Ativan etc…). Although these medications can be very effective, they often have significant side effects (drowsiness, depression, constipation). Benzodiazepines can also be difficult to stop once started. One of the most significant mechanisms in which anti-anxiety medications work is through the GABA receptor system.
GABA is an inhibitory neurotransmitter, meaning that it helps to calm the nervous system and muscular skeletal system. Benzodiazepines have a very strong effect on GABA receptors making them effective but also potentially dangerous.
Many nutraceutical compounds activate the GABA pathway but with a gentler effect than benzodiazepines. Pharma GABA (GABA produced by bacteria), Passionflower, St. Johns Wort, Taurine, 5-HTP and CBD all have well documented effects on GABA and Serotonin. At the Toronto clinic we use these compounds successfully in the treatment of anxiety syndromes with less potential for adverse effects.https://pubmed.ncbi.nlm.nih.gov/ 11679026/
Supplementation for Stress
Every single human being experiences stress throughout their life. Stress can be a healthy natural process in the right circumstances and at the right time. Stress becomes pathological when it is experienced chronically and without appropriate instigation. Long lasting stress can have detrimental effects on multiple biological systems including the immune system, endocrine system (hormones) and cardiovascular system. https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC5137920/
There are no specific pharmaceutical interventions in the treatment of stress. Benzodiazepines are the most common class of drug prescribed for debilitating stress and as I mentioned in the section on anxiety, benzodiazepines can have significant side effects and issues with dependency.
Since there is a wide spectrum of factors that can cause stress a “one size fits all” approach is not always effective. The naturopathic approach is fundamentally holistic and therefore takes into account mental, emotional and physical stressors. For instance a change in work schedule may be contributing to sleep disruption, leading to insomnia, poor work performance and nutritional disruption.
Furthermore, there is an entire class of nutritional and herbal supplements called adaptogens. Adaptogens have the ability to modulate cortisol (stress hormone) preventing peaks and dips in cortisol levels throughout the day. Overtime treatment with adaptogens facilitate a more balanced cortisol output avoiding periods of hyperactivity and burnout. To my knowledge there are no pharmaceutical drugs that act in a similar way. Some common adaptogens are: Ashwagandha, Rodiola and Siberian Ginseng. Vitamins like Vitamin C and Magnesium can help support adrenal function further helping the body to avoid burnout in periods of prolonged stress. At the Toronto clinic I use these adaptogenic compounds in conjunction with other treatments to provide a safe and effective treatment plan for chronic stress.
The mind can be treated through the body. Pharmaceutical interventions can be effective but often come with safety concerns around adverse effects and dependancy. There are many safe and effective natural approaches to mental health conditions through supplementation. At my Toronto clinic we specialize in developing an individualized plan to help achieve your mental health goals.
Traumatic brain injury is damage to the brain that is the result of a head injury. Quality of life is greatly diminished for those living with a traumatic brain injury. Even fatal results can occur. As the quantity of study devoted to CBD develops, there is the rise in the query that whether CBD can help in treating brain injury or not. Currently, the research indicates that CBD possesses neuroprotective properties. Such effects can include mitigating the effect of head injuries.
A flexible and effective anti-inflammatory cannabinoid that has few to no adverse effects is known as cannabidiol or CBD. The number of conditions treatable with CBD increases daily with the introduction of fresh scientific information. There is emerging evidence that CBD is starting to be used as a treatment for severe traumatic brain injury.
TBI can happen to anyone who suffers from brain trauma, and it can affect every aspect of life.
What Do We Understand from Traumatic Brain Injury?
Any brain injury merits serious concern. The brain goes through a cascade of reactions after sustaining a significant injury. Inflammation, edema, and immunological activation are included in this list.
Though this is a usual and helpful set of reflexes in response to a break or fracture. Additional neurological damage might result from this set of events.
When brain cells die, the damage to the brain as a whole will soon follow. Common TBI patients include people who have served in the military, professional athletes, and victims of motor vehicle collisions. TBI can have enduring and crippling repercussions, and might manifest emotionally, physically, behaviorally, and socially.
A lot of the time, these impacts are life-altering. As well as cognitive deterioration and impaired motor function, depression and anxiety are common side effects. Severe symptoms among certain people with TBI can also result in seizures. Conventional medicine currently lacks effective treatments for minor TBI, which is an underreported and frequently misdiagnosed condition.
Scientific Evidence Which Says CBD is Effective for TBI
CBD is showing some evidence of usefulness in reducing some of the harmful effects of TBI, specifically in the areas of inflammation and neurological complications.
A paper published in Frontiers in Pharmacology claims that “The Endocannabinoid System Possesses Potentially Drugable Receptor and Enzyme Targets for the Treatment of Varying TBI Pathology.”
In addition, there are numerous studies which suggest that in combination with THC, CBD is neuroprotective, indicating that regular ingestion of cannabinoids reduces the likelihood of a catastrophic brain injury.
More and more research about TBI is becoming available with each passing year. A variety of research studies agree that the ECS plays a major role in the development of mental, bodily, and behavioral responses after a TBI.
Although further study is needed to produce precise protocols that may be accessible and recommended by mainstream medicine, some preliminary research has already been done. Each example is adding information to the outlook for the condition treated with cannabinoids.
Anecdotal Support for Using CBD as a Treatment for Brain Injury
It takes years for new scientific information to be studied and released. To draw a conclusion, you first must subject the drug being investigated, in this case CBD, to rigorous testing.
While scientific studies take time, evidence exists for the benefits of cannabis in treating brain injury based on anecdotes from patients.
CBD has the potential to improve the quality of life for people who have suffered a brain injury by allowing them to increase their quality of life.
Final Words
CBD’s brain-healing qualities are not yet fully understood and must be investigated further. Much research is being conducted regularly, and soon we will get a clearer understanding of the role of CBD in TBI. The current research suggests that CBD has some properties which can help increase quality of life in brain injury, but we cannot be sure how effective it is or if it has any side effects. We have to wait for more research to be conducted and results to be announced; only then can we be sure about how effective it is to use CBD as a treatment for brain injury.
About the author:

Sean Roberts is a writer by profession. He is a full time writer working with NY Marijuana Card, a leading clinic that provides medical marijuana recommendations. He aims at educating people about the medicinal use of cannabis https://nymarijuanacard.com/
By: Dr. Shawn Meirovici N.D.
Intro
As a cannabis educator and naturopathic doctor I naturally get asked several questions about cannabis. Specifically cannabidiol (CBD) and epilepsy. I believe CBD enriched cannabis oil can be an effective and safe first or second line therapy for various forms of epilepsy and this is why.
Back Story on CBD and Epilepsy
Allow me to first tell you a bit about the story behind CBD and epilepsy. The potential of CBD as a therapeutic option in treating epilepsy came to the forefront back in 2013. Renowned CNN medical journalist Dr. Sanjay Gupta did a special report series on cannabis called “Weed”. One of these episodes highlighted a 5 year old girl named Charlotte Figi.
Charlotte, who had been diagnosed with a severe form of epilepsy called Dravet Syndrome, was being treated with a concentrated CBD oil. Dravet syndrome is characterized by prolonged and frequent seizures that typically begin in the first year of life. Without successful treatment, Dravet can lead to severe health concerns including developmental disabilities. After several anti-epileptic drugs failed to control her seizures, Charlottes family had began to research alternative options to help their daughter.
A little known fact is that CBD was actually discovered and researched before the most famous of the cannabinoids, delta-9 tetrahydrocannabinol (THC). Not too long after the discovery of CBD, research into the calming effects of CBD on the neurological system and its potential as an anti-epileptic came to surface.
One such study came from the Journal of Clinical Pharmacology. Published in 1981, the study found that cannabidiol was effective in almost all epileptic patients (secondary generalized epilepsy) at a dose of 200-300mg daily for 4.5 months. There were no psychological or physical symptoms suggestive of psychotropic or toxic effects. (1)
The Figi’s soon came across some of this research and began searching for high CBD strains of cannabis (not easily attainable at the time). They came across the Stanley Brothers in Colorado who had bred a high CBD low THC strain of marijuana known as “Hippie’s Disappointment”. The name suggesting its low THC content and little to no psychotropic effects.
Charlottes parents and physician said that she experienced a reduction of her epileptic seizures after her first dose of CBD oil! The strain was then renamed “Charlotte’s Web” and thus began a flurry of interest into cannibidiol and changing of marijuana laws across America.
More recently there have been several high quality clinical trials, including three phase 3 clinical trials in 2017. These trials demonstrated the efficacy of cannabidiol in reducing convulsive seizure activity; specifically in children with treatment-resistant Dravet syndrome and Lennox-Gastaut syndrome. (2)

Dr. Sanjay Gupta M.D. CNN Special Report “Weed”
How CBD works
I will now explain how we think CBD works in convulsive syndromes. In order to do so I must first briefly explain an important biological system that all humans, in fact all creatures with the exception of insects, possess called the Endocannabinoid System (ECS). The ECS regulates many bodily systems to maintain balance. One such job of the ECS is to function as a self-regulating harm reduction system; essentially acting as a breaker system shutting down power when circuits get overloaded.
The ECS is able to do this via chemical messengers in our body called endocannabinoids (Cannabinoids found within our body). The two main endocannabinoids are Anandamide (AEA) and 2-Arachidonoylglycerol (2-AG). Endocannabinoids are released at the postsynaptic neuron (the receiving end of a chemical signal). Through retrograde inhibition (a feedback loop) can turn off or quiet a signal. As you can imagine, if there was no off switch things would go haywire very quickly.
Circling back to epilepsy, one of the ways the ECS functions is by maintaining homeostasis in the nervous system. The ECS is involved in the prevention of excess neuronal activity as is the case with a convulsive seizure. So you may now be wondering how CBD fits into this picture.
Our ECS is activated via receptors called cannabinoid receptors. We have many types of these receptors throughout our body. Our endocannabinoids (AEA and 2-AG) as well as phytocannabinoids (cannabinoids from plants such as THC) activate these receptors. Unlike THC, however, CBD does not fit well into our cannabinoid receptors. CBD instead boosts the activity of our endocannabinoids (AEA and 2-AG) by slowing their enzymatic breakdown.
In short, CBD can increase our endocannabinoid tone by inhibiting re-uptake. Much like how an antidepressant boosts serotonin activity by inhibiting re-uptake of serotonin.
There are many other physiological actions of CBD, such as being a potent anti inflammatory and having antidepressant effect. However, for the purposes of understanding how it can work in epilepsy, CBD is thought to act by increasing endocannabinoid tone in the nervous system.
CBD is regarded as a very safe medicinal substance as it doesn’t directly stimulate our receptors, as do many other drugs. Rather, it boosts our own innate endocannabinoid activity.
CBD Safety In Epilepsy
CBD is a generally well tolerated medication, and has no known toxicity (we’re not sure if its even possible to overdose from it). There are however some things that are important to point out to patients considering using CBD, especially when it comes to epileptic patients already taking other anti epileptic drugs (AED).
A randomized control trial (RCT) from 2018 in the journal of Neurology aimed to evaluate the safety of CBD in children with Dravet syndrome. The patients were aged 4-10 years and they received a CBD oil at relatively high doses (5, 10 or 20mg/kg/day). That equates to 65mg per day on the lower end and 260mg per day on the higher end for a 30lb child.
Considering the average adult using CBD consumes somewhere between 20-60mg per day, that’s a pretty hefty dose for a child. The results of the study indicated that for the most part CBD had no effect on other AEDs’ (Clobazam, Valproate, Levetiracetam, Topiramate and Stripentol). There was one exception with N-desmethylclobazam in which it increased levels of this drug. This effect is likely due to how CBD can slow down liver metabolism via a specific enzyme called CYP450. (3)
There was also an increase in liver enzymes in 6 patients taking both valproate and CBD. Something that may not be of much clinical significance but should be monitored. Most of my medicated patients with epilepsy are prescribed Keppra (Levetiracetam) as a first line therapy. It’s good to know that even at high doses (260mg/day) CBD is not likely to interact with this medication. Valproate is the second most common AED that I see clinically. In these patients it is recommended to test the liver enzymes every so often.
There were more adverse effects (AE) in those patients taking CBD as compared to placebo. The most common AEs’ being pyrexia, somnolence, decreased appetite, sedation, vomiting, ataxia and abnormal behaviour. In general CBD was well-tolerated. To compare, the most common AEs’ in patients taking Keppra (Levetiracetam) are: headache, increased blood pressure, somnolence, drowsiness, fatigue, anorexia, weakness, nasopharyngitis and cough. Keppra is also one of the more well tolerated AEDs’. In my opinion CBD, at the very least, is very similar to Keppra in safety profile and efficacy and should therefore be considered as a first or second line therapy.


CBD Efficacy in Epilepsy
One of the more recent studies looking into CBD and epilepsy was conducted just down the street from me at the Hospital for Sick Kids (a world renowned children’s hospital in Toronto Canada).
The study was published in the Annals of Clinical Translational Neurology in August of 2018. What was even more exciting is that the study used a CBD enriched cannabis oil from a licensed producer (Tilray) that many of my patients have access to. The CBD oil contained 100mg/ml CBD and 2mg/ml THC. Nineteen children with Dravet syndrome received the CBD oil for the complete 20-week intervention. The average dose was 13.3mg/kg/day (right in line with the dose of previously discussed safety study). The most common AEs’ were: somnolence, anorexia and diarrhea. Liver enzymes increased in patients also taking Valproate (so it looks like the interactions and adverse effects are pretty consistent).
There was a statistically significant improvement in quality of life, reduction in EEG spike activity (correlated with seizure activity), an average motor seizure reduction of 70.6% (motor seizure reduction rate in Keppra is around 37%) with a 50% responder rate of 63% (comparable to Keppra). (4)(5) Click Here for Sick Kids Study

CBD as first line therapy in Epilepsy
At this point you may be wondering why CBD is not generally considered as a first line therapy option for convulsive seizure disorders?
The reality is that the medical system in North America is generally very conservative in accepting new treatments. This is often a good thing (protecting the public from potentially dangerous or useless medications). However, on the flip side it can be a obstacle for getting naturally derived medicines, that we know to be safe and likely effective, to the patients that would benefit from them.
Currently we only have studies using CBD oil or CBD enriched cannabis oil (Containing other cannabinoids like THC) in patients with severe forms of epilepsy, or who have failed to see benefit with several other AEDs’. However, if we take into account all the information we do have on CBD, we can draw some pretty solid conclusions about its safety profile, the potential adverse effects, interactions with other drugs and its efficacy.
Until we see a robust amount of research using CBD as a first line therapy in a wider array of seizure disorders it is not likely to be accepted as a first or second or third choice by many neurologists. As a Naturopathic Doctor and cannabis educator I do see the potential of CBD for epilepsy. I will therefore continue to advocate for CBDs’ consideration as a first or second line therapeutic agent in many of my patients with epilepsy.
Check out my other articles on CBD and medical marijuana
Epilepsy Foundation stance on medical marijuana

References
- Carlini EA, Cunha JM. Hypnotic and antiepileptic effects of cannabidiol. J Clin Pharmacol. 1981;21(S1):417S-427S. doi:10.1002/j.1552-4604.1981.tb02622.x
- O’Connell, Brooke (May 1, 2017), “Cannabinoids in treatment-resistant epilepsy: A review.”, Epilepsy Behav, Epilepsy & Behavior, 70, 6, 341-348, 70: 341–348, doi:10.1016/j.yebeh.2016.11.012, PMID 28188044
- Devinsky O, Patel AD, Thiele EA, et al. Randomized, dose-ranging safety trial of cannabidiol in Dravet syndrome. Neurology. 2018;90(14):e1204-e1211. doi:10.1212/WNL.0000000000005254
- McCoy B, Wang L, Zak M, et al. A prospective open-label trial of a CBD/THC cannabis oil in dravet syndrome. Ann Clin Transl Neurol. 2018;5(9):1077-1088. Published 2018 Aug 1. doi:10.1002/acn3.621
- Abou-Khalil B. Levetiracetam in the treatment of epilepsy. Neuropsychiatr Dis Treat. 2008;4(3):507-523. doi:10.2147/ndt.s2937
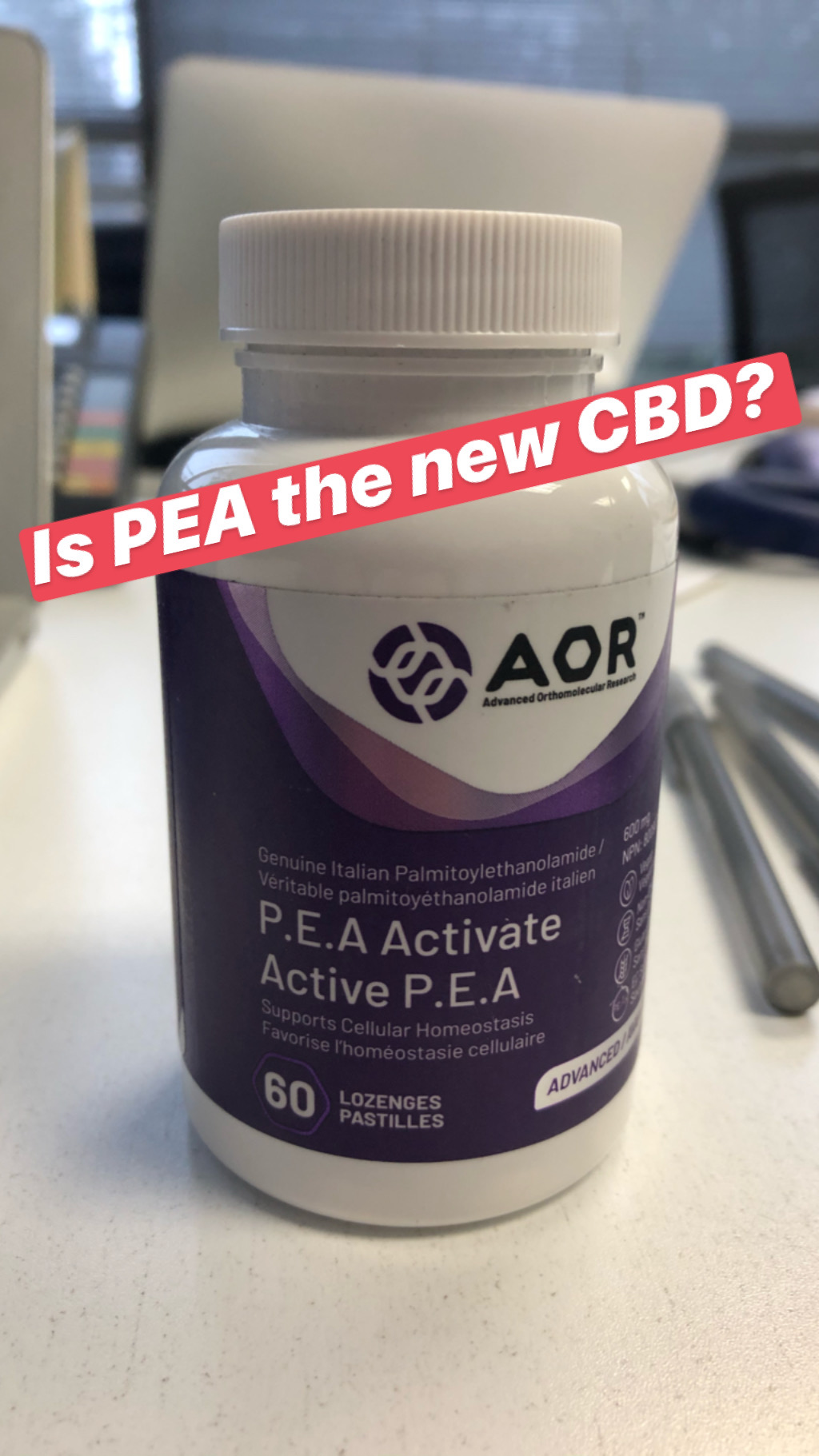
It was my hope to find an effective alternative to Cannabidiol (CBD) that wouldn’t land me in jail when I travel; so is PEA the new CBD?
PEA stands for Palmitoylethanolamide. It is a fatty acid that is found in Eggs, Cheese, Meats and Peanuts. We also make PEA during stress, infections, inflammation, trauma, allergies, pain, cardiac disease, kidney disease and obesity. Much like our endocannabinoids, PEA is responsible for maintaining cellular homeostasis.

How does it work?
While PEA does not have a direct effect on Cannabinoid receptor (CB1 and CB2) it does have similar mechanisms of action to our endocannabinoids and cannabidiol (CBD). PEA looks very similar to our body’s own endocannabinoids (AEA and 2-AG). These similarities allow PEA to exert effects similar to our AEA and 2-AG.

PEA down regulates mast cells, which are responsible for the release of histamine and other inflammatory mediators. PEA can therefore be a powerful molecule for immune heath, inflammation, pain, neuro-protection and allergies. PEA has direct action on receptors GPCR55 and GPR119, which produce effects similar to activation of CB1 and CB2 by endocannabinoids, THC and CBD. PEA also acts similarly to CBD by affecting the breakdown of endocannabinoids via inhibition of the enzymes FAAH and MAGL.

The Research
Several studies have shown that when PEA is used with opioid type drugs for low back pain, the dose of the opioids could be reduced significantly. PEA was found to exert pain relief animal models of inflammation and neuropathic pain. These analgesic effects are thought to be due to increasing endocannabinoid levels similarly to how CBD works. All in all many studies have revealed that PEA exerts similar effects to CBD. So I thought I would give this supplement a whirl, as a alternative to CBD (especially for travel) would be an important option for patients using CBD.
My 5-day Trial with PEA
I took the supplement P.E.A. Activate from AOR , which contains 600mg PEA per lozenge. My daily dose was two lozenges per day and I did that for 5 days. I noticed a strange light-headed feeling about 5 minutes after chewing my first lozenge. The feeling lasted for a bout 30min. I was excited that I actually felt a bit different after that fist dose by unfortunately each dose produced a similar effect (a light relaxing feeling) that only lasted between 30-60min. There didn’t seem to be much carry over from one dose to another. The effects were always pretty fast acting but short-lived. Furthermore I had a return of some muscle soreness that was absent for most of the time that I was taking my CBD supplement. So, it seemed like, for me, the PEA was not having the same effect that I had experienced while on CBD.
In summary, the effects that I experienced during my PEA trial were fast acting but short-lived. PEA may therefore be a useful tool for acute episodes of anxiety, pain etc… but it did not have the same accumulative and long term effects that I experienced with CBD. The research on PEA is compelling and it is possible that this supplement warrants a more long-term trial. According to the research PEA seems to be a potential alternative to CBD but from my experience it falls a bit short. Check out my video review of PEA here.
My review of Ruxton by Broken Coast. Deeply relaxing, very potent 4 out of 5 stars.