An Introduction to NAFLD
Non-alcoholic fatty liver disease (NAFLD) is more than just a medical term; it’s a growing health concern that’s capturing the attention of health enthusiasts, medical professionals, and patients alike. With its rising prevalence, it’s crucial to understand what NAFLD entails and why it’s being increasingly recognized as a major health issue.
NAFLD refers to a range of liver conditions affecting individuals who drink little to no alcohol. It’s characterized by an excess accumulation of fat in the liver. Unlike alcoholic liver disease, NAFLD occurs in people who consume minimal or no alcohol, making it somewhat paradoxical. This distinction is important and underscores the need for awareness and understanding.
Statistics reveal a concerning trend; NAFLD is one of the most common liver disorders globally. In the United States alone, it’s estimated that about 25% of adults are living with this condition. With such widespread prevalence, it’s no wonder that awareness and education about NAFLD are more important than ever.

Understanding the Causes
Grasping the causes of NAFLD is vital for both prevention and management. At the heart of NAFLD lie several primary causes and risk factors that contribute to its development. The most common culprits include obesity, insulin resistance, and metabolic syndrome.
Obesity is a significant driver of NAFLD, with excess body weight leading to fat accumulation in the liver. This is particularly concerning given the global obesity epidemic. Insulin resistance, often associated with type 2 diabetes, is another key factor. It disrupts the body’s ability to regulate sugar and fat metabolism, contributing to liver fat buildup.
Genetic predisposition also plays a role in NAFLD susceptibility. Certain genetic variations can increase the risk of developing this condition. These genetic factors, combined with lifestyle choices, create a complex web of influences that can lead to NAFLD. Understanding these factors is crucial for those seeking to mitigate their risk.
Symptoms and Diagnosis
Recognizing the symptoms of NAFLD can be challenging because it often presents with few, if any, noticeable signs. Many individuals with NAFLD remain asymptomatic, making early detection difficult. When symptoms do appear, they can include fatigue, discomfort in the upper right abdomen, and unexplained weight loss.
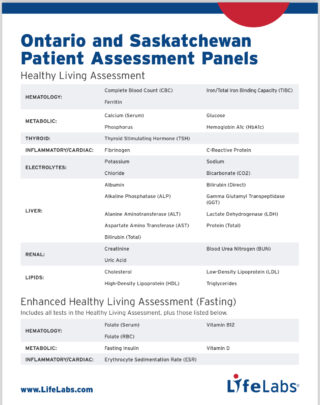
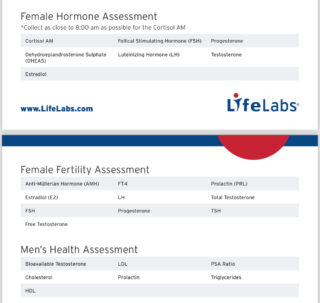
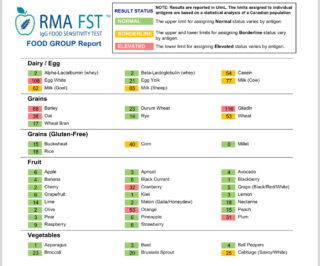
Diagnosing NAFLD involves a series of tests and evaluations. Physicians typically start with blood tests to assess liver function and rule out other liver conditions. Imaging studies, such as ultrasound or MRI, can help visualize fat accumulation in the liver. In some cases, a liver biopsy may be necessary to confirm the diagnosis and assess the extent of liver damage.
Early diagnosis is crucial for preventing the progression of NAFLD to more severe liver conditions. Regular check-ups and vigilance for risk factors can aid in catching the disease before it advances. Patients should work closely with healthcare providers to monitor liver health and implement appropriate management strategies.
Complications of NAFLD
While NAFLD itself may not always cause immediate harm, its potential complications are concerning. One of the most serious complications is non-alcoholic steatohepatitis (NASH), an aggressive form of fatty liver disease. NASH can lead to inflammation, liver cell damage, and fibrosis, significantly increasing the risk of liver cirrhosis.
Cirrhosis, a condition where healthy liver tissue is replaced by scar tissue, is a grave consequence of untreated NAFLD. It can impair liver function, leading to liver failure and an increased risk of liver cancer. Understanding these potential outcomes underscores the importance of early intervention and vigilant management of NAFLD.
Complications of NAFLD extend beyond the liver. Research suggests that individuals with NAFLD are at a higher risk of cardiovascular disease and type 2 diabetes. These associations highlight the interconnectedness of metabolic health and emphasize the need for comprehensive care.

Treatment and Management
Managing NAFLD requires a multi-faceted approach that addresses both lifestyle changes and medical interventions. One of the most effective strategies is weight loss, which can significantly reduce liver fat and improve liver function. A combination of diet and exercise is often recommended to achieve and maintain a healthy weight.
Dietary modifications play a crucial role in managing NAFLD. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce liver fat. Some studies suggest that intermittent fasting and omega-3 fatty acids might have positive effects on liver health. Consulting a healthcare provider or registered dietitian can provide personalized guidance.
Medical treatments for NAFLD are still evolving. While there are no specific medications approved for NAFLD, some treatments target underlying conditions like diabetes or high cholesterol. Clinical trials are ongoing to explore new therapeutic options. Patients should work closely with their healthcare providers to develop a tailored management plan.

Prevention of NAFLD
Prevention is the best strategy when it comes to NAFLD. Adopting a healthy lifestyle can significantly reduce the risk of developing this condition. Maintaining a balanced diet, engaging in regular physical activity, and managing weight are essential steps in prevention.
Dietary choices play a critical role. Reducing the consumption of saturated fats and sugars can help prevent liver fat accumulation. Incorporating foods with anti-inflammatory properties, such as garlic and curcumin, into the diet may also offer protective benefits.
Regular exercise is equally important. Engaging in aerobic activities like walking, jogging, or cycling can improve insulin sensitivity and promote weight loss. Combining exercise with strength training can further enhance metabolic health and prevent NAFLD.
The Future of NAFLD
The future of NAFLD management holds promise as research continues to uncover new insights and treatments. Scientists are exploring novel approaches, including advanced imaging techniques and biomarkers, for early detection and monitoring of NAFLD. These advancements could revolutionize how we diagnose and manage this condition.
Pharmaceutical research is also making strides in developing targeted therapies for NAFLD. Some medications are showing promise in clinical trials, offering hope for more effective treatment options in the future. These breakthroughs have the potential to change the landscape of NAFLD management.
Public health initiatives are essential in raising awareness and promoting prevention strategies for NAFLD. Education campaigns and community outreach programs can empower individuals to make informed lifestyle choices. Collaborative efforts between healthcare providers, researchers, and policymakers are crucial for tackling this growing health challenge.
Conclusion
In conclusion, NAFLD is a prevalent and potentially serious liver condition that affects millions worldwide. Understanding its causes, symptoms, complications, and management options is essential for individuals seeking to protect their liver health. By adopting a healthy lifestyle, engaging in regular check-ups, and staying informed about the latest research, we can all take proactive steps to combat NAFLD.
For those living with or at risk of NAFLD, it’s important to remember that you’re not alone. Support from healthcare providers, family, and friends can make a significant difference in managing this condition. Together, we can raise awareness, promote prevention, and encourage healthier lives.
Next Steps
If you or someone you know is concerned about NAFLD, take action today. Share your experiences, ask questions, and seek professional advice for any health concerns. Together, we can work towards better liver health and a brighter future for all.