Ensuring optimal health and wellness requires a proactive approach. As a healthcare provider, I always recommend a series of comprehensive tests and panels for all new patients. These tests offer invaluable insights into various aspects of your health, enabling personalized care and early detection of potential issues. Here are my top five recommended tests and panels:
1. LifeLabs: Enhanced Healthy Living Assessment Panel
Overview:
The Enhanced Healthy Living Assessment Panel from LifeLabs is a comprehensive screening tool designed to offer a holistic view of your overall health. It includes a broad spectrum of tests that evaluate critical factors such as blood glucose levels, cholesterol, liver function, kidney function, and more.
Why It’s Crucial:
This panel serves as a foundational health check, identifying any imbalances or abnormalities that could affect your long-term wellness. By getting a detailed snapshot of various biomarkers, we can tailor a health plan specifically designed for your needs.
What It Tests For:
- Complete Blood Count (CBC)
- Lipid Profile (Cholesterol, LDL, HDL, Triglycerides)
- Liver Function Tests (ALT, AST, ALP, Bilirubin)
- Kidney Function (Creatinine, eGFR)
- Blood Glucose Levels
- Vitamin D
- Vitamin B12
Benefits:
- Early detection of health issues
- Comprehensive understanding of your current health status
- Benchmark data for future comparisons
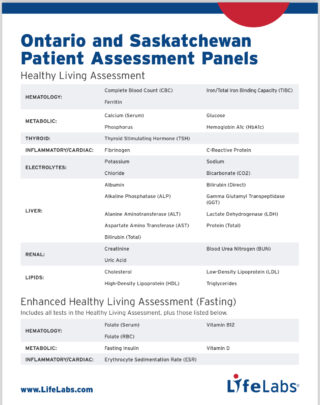
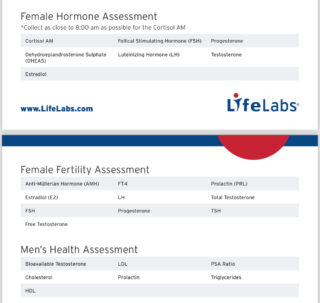
2. LifeLabs: Female/Male Hormone Panel
Overview:
Hormones play a pivotal role in regulating numerous bodily functions, including metabolism, reproductive health, and mood. The Female/Male Hormone Panel from LifeLabs is designed to assess hormone levels, helping to identify imbalances that could be affecting your health.
Why It’s Crucial:
Hormonal imbalances can lead to a variety of health issues, including fatigue, weight gain, mood swings, and fertility problems. This panel provides a detailed analysis of key hormones, enabling targeted interventions that can help restore balance.
What It Tests For:
- Testosterone
- Estrogen (Estradiol)
- Progesterone
- Cortisol
- Thyroid-Stimulating Hormone (TSH)
Benefits:
- Identification of hormonal imbalances
- Personalized treatment plans for hormonal health
- Improved overall well-being
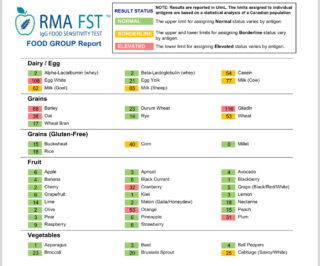
3. RMA: Food Sensitivity IgG Panel
Overview:
The Food Sensitivity IgG Panel from Rocky Mountain Analytical (RMA) tests for IgG antibodies to identify potential food sensitivities. Unlike immediate allergic reactions (IgE), IgG-mediated reactions can cause delayed symptoms, making them harder to pinpoint.
Why It’s Crucial:
Food sensitivities can lead to chronic inflammation, digestive issues, and other health problems. Identifying and eliminating trigger foods can significantly improve your quality of life and alleviate a range of symptoms.
What It Tests For:
- Over 200 common foods, including dairy, grains, nuts, fruits, and vegetables
Benefits:
- Identification of trigger foods causing adverse reactions
- Alleviation of chronic symptoms like bloating, headaches, and fatigue
- Enhanced digestive health and overall well-being
4. LifeLabs: Apolipoprotein B
Overview:
Apolipoprotein B (ApoB) is a protein involved in lipid metabolism and is a key marker for cardiovascular risk. Elevated ApoB levels are associated with an increased risk of atherosclerosis and heart disease.
Why It’s Crucial:
Traditional lipid profiles may not provide a complete picture of cardiovascular risk. Measuring ApoB offers a more accurate assessment, particularly for individuals with normal LDL cholesterol but still at risk for heart disease.
What It Tests For:
- Apolipoprotein B levels
Benefits:
- More accurate cardiovascular risk assessment
- Personalized strategies for heart disease prevention
- Improved cardiovascular health
5. Mosaic Diagnostics: Organic Acids Test
Overview:
The Organic Acids Test (OAT) from Mosaic Diagnostics examines metabolic byproducts in urine, offering insights into various aspects of your health, including mitochondrial function, neurotransmitter levels, and gut health.
Why It’s Crucial:
OAT provides a comprehensive overview of metabolic health, identifying issues that might not be apparent through traditional blood tests. It can uncover underlying factors contributing to chronic conditions, fatigue, and mood disorders.
What It Tests For:
- Metabolic markers
- Neurotransmitter metabolites
- Gut dysbiosis markers
- Vitamin and mineral deficiencies
Benefits:
- Identification of metabolic imbalances
- Tailored nutritional and lifestyle interventions
- Enhanced energy levels and mental clarity

Conclusion
These top five tests and panels offer a thorough examination of key health areas, providing a solid foundation for personalized care. By investing in these assessments, you are taking proactive steps toward achieving optimal health and well-being.
Ready to take control of your health? Schedule your tests today and embark on a journey toward a healthier, happier you. Feel free to reach out if you have any questions or need further guidance.
Call to Action
For more information or to book your tests, contact us at s.meirovici@physio-logic.com or call 416-490-8243 . Your health is our priority!